Quantative computerized tomography assessment of lung density as a predictor of postoperative pulmonary morbidity in patients with lung cancer
Introduction
Lung cancer is one of the most common malignant neoplasm and leading causes of death from cancer worldwide. Surgical resection is the best treatment for early stage of non small cell lung cancer (NSCLC) (1). Emphysema is defined as the pathological air space enlargement beyond the terminal respiratory bronchioles. Both emphysema and lung cancer can arise from biological damage caused by smoking (2,3). Mean lung density measurement was formerly described in the follow-up of the emphysema progression and monitoring the effect of therapeutic interventions. Also there are too many scientific publications about the correlation of quantitative measurements of lung volumes with computed tomography (CT) and pulmonary function tests (4-6). In a recent study, the authors have found that CT densitometry and histological grading of emphysema were well correlated within the variation of pulmonary function in patients undergoing lobectomy for lung cancer. Additionally they have found lower reduction of pulmonary function after lobectomy in patients with a higher degree of emphysema (7). The aim of our study was to assess the correlation between volume of emphysema, mean lung density measured from the preoperative CT scans and postoperative morbidity.
Materials and methods
Fifty consecutive patients with NSCLC who underwent lobectomy/segmentectomy between February 2013 and March 2014 were enrolled retrospectively in this study. Exclusion criteria were pleural effusion, segmental or lobar atelectasis, bullae larger than 3 cm, previous, lobectomy, segmentectomy or pneumonectomy operations, fibrosis detected in the CT images. To standardize the surgical procedure we enrolled only the patients who have lobectomy or segmentectomy in the study.
Postoperative complications were defined as those occurring within 30 days of thoracotomy. Pneumonia: fever bigger than 38 °C for 48 hours, radiological evidence including atelectasis and documentation of pathological organism culture. Lobar atelectasis: atelectasis due to mucus plugging, evidenced on chest radiograph and requiring bronchoscopy. Pleural effusion: pleural effusion evidenced on chest radiograph or CT scan and requiring chest tube placement. Prolonged air leak: air leak requiring >7 days of postoperative chest tube drainage. This study was approved by the ethical committee of our institution.
Computed tomography (CT)
All CT images were produced in a multi detector row CT machine (MDCT). Peak kilovolt was 120 kV for all studies and automatic tube current modulation was allowed to change the milliampere for each slice to optimize the exposure for cross sectional thickness of the patient chest. Noise index was between 14 and 16.1. Slice thicknesses were between 3 to 5 mm for spiral mode with standard kernel and 1.25 to 2.5 mm for high resolution mode and appropriate kernel for each make of MDCT. Images of chest produced without IV contrast material were preferred for quantitative lung density and volume measurements. All preoperative CT examinations were performed during a breath-hold at deep inspiration and the same reconstruction algorithm used for CT images in all patients.
Emphysema calculation of lung CT images
All lung images were loaded and evaluated in a dedicated workstation (Advantage Workstation 4.2, General Electric Healthcare, USA). Images reconstructed after thresholding between −400 and −1,024 HU to remove the densities of other thoracic parts than air filled lung densities. Trachea, main bronchi and other gas containing structures nearby like stomach and colon were removed manually by “remove object” function of the software. A histogram was created after pure lung density volume model was obtained. Whole lung volume, mean lung density, and standard deviations were recorded for each patient. Emphysematous lung volume was measured by relocating the minimum lung density bar from −400 to −900 HU on histogram image. Average lung density for emphysematous lung volume, percentage to total lung volume and standard deviation were recorded again. Each lung volume was measured in addition by removing the right lung volume manually and repeating the procedure above for the left lung.
Pulmonary function tests
In all patients, forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and diffusion capacity of lungs for carbon monoxide (DLCO) were analyzed preoperatively in a standardized attitude (Vmax Encore system, Germany).
Statistical analyses
Statistical analyses were done using IBM SPSS Statistics v 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk NY, USA). Results are presented as mean ± SD. Testing for normally distributed continuous data was done using student t-test. Non-normally distributed data were analyzed with Mann-Whitney U-test. Spearman correlations were assessed between the variables.
Receiver operating characteristic (ROC) curve, Youden index and area under the curve (AUC) were calculated to test the effectiveness of lung density and emphysematous volume to predict postoperative pulmonary morbidity. The factors affecting postoperative pulmonary morbidity were evaluated with univariate analyses and in case of P<0.25 the factors also evaluated with multivariate logistic regression analyses. A P value less than 0.05 was noted as statistically significant.
Results
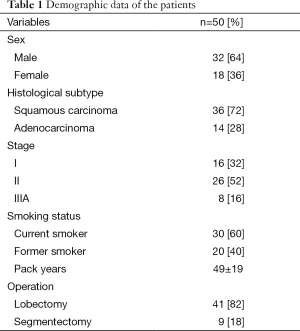
Fifty patients (32 males, 18 females with a mean age of 54.4±13.9 years) who were operated for lung cancer constituted the study population. Forty percent of the patients were ex-smokers whereas 60% were current smoker and the mean pack-years smoked were 49±19 years. All resections were performed through a postero-lateral thoracotomy. Twenty patients had lower lobectomy, 18 patients had upper lobectomy and three patients had middle lobectomy. All segmentectomies were done from the lower lobe (Table 1). There was no operative mortality. Also the type of surgery did not affect the pulmonary morbidity (P=0.2).
Full table
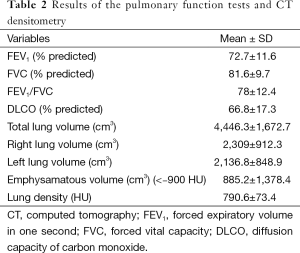
Twenty four pulmonary complications were occurred in 16 patients postoperatively: pneumonia (n=2), lobar atelectasis (n=8), pleural effusion (n=4), prolonged air leak (n=10). There were no statistically significant differences between gender regarding age, pulmonary function parameters, and quantitative measurements of the lungs (P>0.05). Mean FEV1 (% of predicted), mean FVC (% of predicted) and mean DLCO (% of predicted) were 72.7%±11.6%, 81.6%±9.7%, and 66.8%±17.3% respectively. Mean total lung volume was 4,446.3±1,672.7 cm3; mean total lung density was −790.6±73.4 HU. The volume of emphysematous lung was (<−900 HU) 885.2±1,378.4 cm3 (Table 2).
Full table
FEV1 (r=−0.494, P=0.02) and DLCO (r=−0.643, P<0.001) were found to be correlate with the volume of emphysematous lung. Furthermore FEV1 (r=0.59, P<0.001) and DLCO (r=0.48, P<0.001) were also found to be correlate with mean lung density.
A comparison was done between pulmonary morbidity and quantitative CT analysis of lung parenchyma and spirometric findings. Postoperative pulmonary morbidity was found to be significantly high in patients with lower density (P<0.001), with higher volume of emphysema (P<0.001) and with lower preoperative DLCO (P=0.039). However there was no correlation between preoperative FEV1 and pulmonary morbidity (P=0.09).
When we looked at the correlation of quantitative CT measurements with each pulmonary complication, pneumonia (P=0.015), lobar atelectasis (P=0.02), pleural effusion (P=0.03) and prolonged air leaks (P<0.001) were found to be significantly high in patients with lower density. Furthermore pneumonia (P=0.02), lobar atelectasis (P=0.012), pleural effusion (P=0.011), and prolonged air leaks (P<0.001) were found to be significantly high in patients with higher volume of emphysema.
We determined centrilobular emphysema in 13 patients, panlobular emphysema in six patients and paraseptal emphysema in six patients and we could not determine emphysema by visual CT evaluation in 25 patients. There was no correlation between emphysema subtype and pulmonary morbidity (P=0.311). Emphysema was mainly observed in the upper lobes in 18 patients. In seven patients emphysema was extensive. The emphysema was heterogeneous in all patients. Also there was no correlation between the distribution of emphysema and pulmonary morbidity (P=0.4).
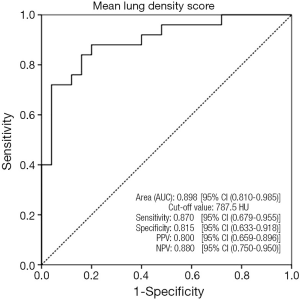
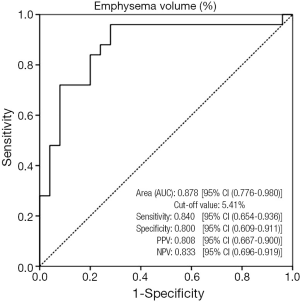
Analysis of the ROC curve showed an AUC of 0.898 [95% confidence interval (CI), 0.810-0.985, P<0.001] for lung density predicting postoperative pulmonary morbidity with an optimal cut-off value of 787.5 HU. The sensitivity and specificity for the cut-off value of density were 86.96% and 81.48% (kappa =−0.68, P<0.001) respectively. The positive predictive value and negative predictive value for the cut-off value of density were 0.80 (95% CI, 0.659-0.896) and 0.88 (95% CI, 0.750-0.950) respectively (Figure 1). Additionally a cut-off point of 5.41% for emphysematous volume showed 84.00% (95% CI, 0.654-0.936) sensitivity and 80.00% (95% CI, 0.609-0.911) specificity for predicting the pulmonary morbidity (kappa =0.64, P<0.001). The AUC value for emphysematous volume was 0.878 (95 CI, 0.776-0.980, P<0.001). The positive predictive value and negative predictive value for the cut-off value of emphysematous volume were 0.81 (95% CI, 0.667-0.901) and 0.83 (95% CI, 0.696-0.919) respectively (Figure 2).
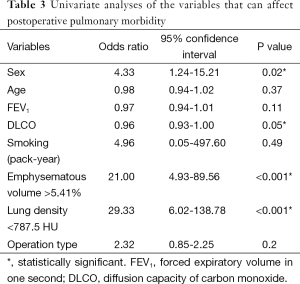
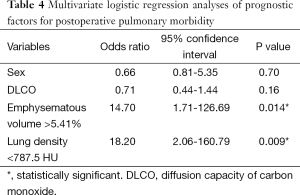
According the univariante analyses sex (P=0.022), lung density 5.41% (P<0.001) were affecting the postoperative pulmonary morbidity (Table 3). Among these significant variables evaluated by univariate analyses, independent prognostic factors of postoperative pulmonary morbidity as determined by multivariate analyses were lung density 5.41% (P=0.014) (Table 4).
Full table
Full table
Discussion
Emphysema is anatomically defined as an abnormal permanent enlargement of the air space distal to the terminal bronchioles (8). CT densitometry is frequently used to evaluate the extent and severity of parenchyma destruction in chronic pulmonary emphysema (9). Anatomical lung resection is still the only curative treatment in patients with localized disease of NSCLC and this treatment option is associated with morbidity of 12-50% and mortality of 2-12% (10).
The most significant risk factor for both emphysema and lung cancer in the developed countries is cigarette smoking. Emphysema is the most common coexisting lung disease in patients with lung cancer and it generally cause postoperative pulmonary morbidity after lung resection (11). CT of chest is the primary modality to stage lung cancer and to detect the candidates for surgical resection. Also quantitative measurements of lungs could have done from the preoperative CT without incurring additional costs (12,13).
Quantitative CT scanning has been studied to determine the severity of the emphysema and it may reflect the volume of functioning pulmonary tissue more precisely. It is also superior to spirometry to detect the early stage emphysema (14,15). There are several reports concerning about the value of quantitative CT to predict the pulmonary function after lung cancer surgery. Their findings indicate that quantitative CT has a better potential for predicting the postoperative pulmonary functions than spirometric measurements. It also shows good agreement with perfusion scintigraphy (13,16-18).
In a study the authors established a novel means of predicting postoperative hypoxemia by quantitative CT. They stated that quantitative CT was superior to conventional spirometric variables in predicting postoperative hypoxemia (19). In another study the authors found that quantitative CT in combination with spirometric measurements may improve prediction of cardiopulmonary complications in patients undergoing lobectomy for lung cancer (20).
In the current study we have found preoperative FEV1 and DLCO were correlated with mean lung density and emphysematous volume assessed with preoperative CT. We have investigated the correlation of preoperative quantitative CT measurements of lungs with postoperative pulmonary morbidity. Lung density showed a negative correlation with postoperative pulmonary morbidity. On the other hand emphysematous volume measured from the preoperative CT showed a positive correlation with postoperative pulmonary morbidity. According to the ROC analysis an AUC for lung density predicting postoperative pulmonary morbidity was 0.898 with a cut-off value of −787.5 HU. An AUC for emphysematous volume predicting postoperative pulmonary morbidity was 0.878 with a cut-off value of 5.41%. The sensitivity and specificity of both lung density and emphysematous volume for predicting the postoperative pulmonary morbidity were higher than 80%. Additionally our results according to multivariate analyses showed that lung density <787.5 HU and emphysematous volume >5.41% was strong independent prognostic factors for postoperative pulmonary morbidity.
Early changes in lung parenchyma due to cigarette smoking could be detected by quantitative CT measurements before any deterioration in pulmonary functions (21). On CT images attenuation values between −400 to −1,024 HU were considered to limit the lung parenchyma from the surrounding tissues. There are several studies focused on attenuation lower than −900 HU for quantitative assessment of emphysema but on the other hand studies assessing the attenuation higher than −900 HU are rare (22,23). Karimi et al. studied about assessment of lung parenchyma inflammation in current smoker of chronic obstructive pulmonary disease patients and they focused on the areas between −750 and −900 HU representing lung tissues in the denser normal range to quantify the early signs of pulmonary disease. They have found smokers have denser lungs than never smokers and the density in smokers is associated to measures of systemic inflammation and cell concentration in bronchoalveolar lavage (24). In this study 60% of the patients were current smokers and the patients who have a mean density lower than −787.5 HU had a high pulmonary complication rate. This can be explained with arithmetic mean of heterogeneous lung tissue and inflammation in the denser normal range of lung parenchyma due to smoking.
Prolonged air leaks, is the most common postoperative condition that causes a prolonged hospital stay, for patients who undergo pulmonary resections. It is an unwanted complication because it increases risks of pneumonia, empyema, and increases risks of thrombo-embolism due to prolonged hospital stay. Also it has been demonstrated that air leak lasting more than 5 days was associated with greater pulmonary morbidity, such as atelectasis, pneumonia, and empyema (25-28). Emphysema is regarded as a risk factor for developing prolonged air leak in cases where patients with emphysema require an operation (26,29). This is possibly due to underlying lung substrate in patients with emphysema is more easily injured during surgery and takes longer to heal. In our study prolonged air leaks were the most common postoperative complication and it was found to be significantly high in patients with higher volume of emphysema and lower density.
In summary, we suggest that measurements of density and emphysematous volume from the preoperative CT in lung cancer are easy, without extra charges and widely available method seemed to have potential to predict the postoperative pulmonary morbidity.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ginsberg R, Roth J, Fergusson M. Lung cancer surgical practice guidelines. Society of Surgical Oncology practice guidelines. Oncology (Williston Park) 1997;11:889-92, 895.
- Parkin DM, Pisani P, Lopez AD, et al. At least one in seven cases of cancer is caused by smoking. Global estimates for 1985. Int J Cancer 1994;59:494-504. [PubMed]
- Evans MD, Pryor WA. Cigarette smoking, emphysema, and damage to alpha 1-proteinase inhibitor. Am J Physiol 1994;266:L593-611. [PubMed]
- Iwano S, Okada T, Satake H, et al. 3D-CT volumetry of the lung using multidetector row CT: comparison with pulmonary function tests. Acad Radiol 2009;16:250-6. [PubMed]
- Matsuoka S, Kurihara Y, Yagihashi K, et al. Quantitative assessment of air trapping in chronic obstructive pulmonary disease using inspiratory and expiratory volumetric MDCT. AJR Am J Roentgenol 2008;190:762-9. [PubMed]
- Moloney F, McWilliams S, Crush L, et al. CT Densitometry as a Predictor of Pulmonary Function in Lung Cancer Patients. Open Respir Med J 2012;6:139-44. [PubMed]
- Carretta A, Ciriaco P, Melloni G, et al. Correlation of computed tomography densitometry and pathological grading of emphysema with the variation of respiratory function after lobectomy for lung cancer. Interact Cardiovasc Thorac Surg 2010;10:914-7; discussion 917-8. [PubMed]
- Pauwels RA, Buist AS, Calverley PM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001;163:1256-76. [PubMed]
- Cavigli E, Camiciottoli G, Diciotti S, et al. Whole-lung densitometry versus visual assessment of emphysema. Eur Radiol 2009;19:1686-92. [PubMed]
- Nagasaki F, Flehinger BJ, Martini N. Complications of surgery in the treatment of carcinoma of the lung. Chest 1982;82:25-9. [PubMed]
- Mannino DM, Braman S. The epidemiology and economics of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007;4:502-6. [PubMed]
- Madani A, Keyzer C, Gevenois PA. Quantitative computed tomography assessment of lung structure and function in puzlmonary emphysema. Eur Respir J 2001;18:720-30. [PubMed]
- Sanders C, Nath PH, Bailey WC. Detection of emphysema with computed tomography. Correlation with pulmonary function tests and chest radiography. Invest Radiol 1988;23:262-6. [PubMed]
- Quint L, Francis I, Wahl R, et al. Imaging. In: Pass H, Mitchell J, Johnson D, et al, editors. Lung cancer. Philadelphia: Lippincott Williams & Wilkins, 2000:535-78.
- Ueda K, Tanaka T, Li TS, et al. Quantitative computed tomography for the prediction of pulmonary function after lung cancer surgery: a simple method using simulation software. Eur J Cardiothorac Surg 2009;35:414-8. [PubMed]
- Wu MT, Pan HB, Chiang AA, et al. Prediction of postoperative lung function in patients with lung cancer: comparison of quantitative CT with perfusion scintigraphy. AJR Am J Roentgenol 2002;178:667-72. [PubMed]
- Papageorgiou CV, Antoniou D, Kaltsakas G, et al. Role of quantitative CT in predicting postoperative FEV1 and chronic dyspnea in patients undergoing lung resection. Multidiscip Respir Med 2010;5:188-93. [PubMed]
- Ohno Y, Koyama H, Nogami M, et al. State-of-the-art radiological techniques improve the assessment of postoperative lung function in patients with non-small cell lung cancer. Eur J Radiol 2011;77:97-104. [PubMed]
- Ueda K, Kaneda Y, Sudou M, et al. Prediction of hypoxemia after lung resection surgery. Interact Cardiovasc Thorac Surg 2005;4:85-9. [PubMed]
- Ueda K, Kaneda Y, Sudoh M, et al. Role of quantitative CT in predicting hypoxemia and complications after lung lobectomy for cancer, with special reference to area of emphysema. Chest 2005;128:3500-6. [PubMed]
- Remy-Jardin M, Remy J, Boulenguez C, et al. Morphologic effects of cigarette smoking on airways and pulmonary parenchyma in healthy adult volunteers: CT evaluation and correlation with pulmonary function tests. Radiology 1993;186:107-15. [PubMed]
- Newell JD Jr, Hogg JC, Snider GL. Report of a workshop: quantitative computed tomography scanning in longitudinal studies of emphysema. Eur Respir J 2004;23:769-75. [PubMed]
- Gierada DS, Yusen RD, Pilgram TK, et al. Repeatability of quantitative CT indexes of emphysema in patients evaluated for lung volume reduction surgery. Radiology 2001;220:448-54. [PubMed]
- Karimi R, Tornling G, Forsslund H, et al. Lung density on high resolution computer tomography (HRCT) reflects degree of inflammation in smokers. Respir Res 2014;15:23. [PubMed]
- Loran DB, Woodside KJ, Cerfolio RJ, et al. Predictors of alveolar air leaks. Chest Surg Clin N Am 2002;12:477-88. [PubMed]
- Shrager JB, DeCamp MM, Murthy SC. Intraoperative and postoperative management of air leaks in patients with emphysema. Thorac Surg Clin 2009;19:223-31. ix. [PubMed]
- Dexter EU, Kohman LJ. Perioperative care of patients undergoing thoracic surgery. In: Sellke FW, del Nido PJ, Swanson SJ, editors. Sabiston & Spencer Surgery of the Chest. 7th ed. Philadelphia: Saunders, 2004:43-57.
- Okereke I, Murthy SC, Alster JM, et al. Characterization and importance of air leak after lobectomy. Ann Thorac Surg 2005;79:1167-73. [PubMed]
- Abolhoda A, Liu D, Brooks A, et al. Prolonged air leak following radical upper lobectomy: an analysis of incidence and possible risk factors. Chest 1998;113:1507-10. [PubMed]


