Early and sustained blood pressure control is necessary for stroke prevention
Introduction
Hypertension is the most common and most important risk factor for coronary artery disease (CAD), heart failure (HF), chronic kidney failure (CKD), and especially stroke, if left untreated. Stroke is a devastating complication of hypertension and is a major cause of death and disability worldwide and its incidence increases linearly with the blood pressure (BP) and level and the advancement of age (1-3). Lewington et al., have shown that the incidence of stroke was directly related to the level of systolic and diastolic BP (SBP, DBP) for all age groups, but with higher prevalence in older than younger subjects (3). Stroke, besides being a cause of long-term disability for the affected person, it is also a significant burden on society and healthcare expenditures (4). According to this report, each year approximately 795,000 people experience a new or recurrent stroke, with 610,000 being first strokes and 185,000 recurrent strokes with 87% of all strokes being ischemic and 10% being hemorrhagic. The direct and indirect expenditures in the US for the year 2012 were $71.6 billion (4), and it is projected that by the year 2030, the total stroke-related, medical costs to be $183.13 billion, with the majority of the projected increase to arise from those 65-79 years of age (5). Stroke is the third leading cause of death in the in the US after ischemic heart disease (IHD) and cancer. Worldwide in 2010, the prevalence of stroke was 33 million with 16.9 million people having a first stroke and stroke was the second-leading global cause of death behind IHD (6). Possible causes for this increase in stroke incidence are the ageing of the population, the poor control of BP as well as the other cardiovascular risk factors, like obesity, diabetes mellitus and hyperlipidemia (5-7). However, recent studies show that the incidence of ischemic and hemorrhagic strokes has decreased significantly between 1990 and 2010 by 13% and 19% respectively, in high income countries, but not in low to middle income countries (7). This could, possibly, reflect the better control of BP and other risk factors in the high income countries.
Treatment of hypertension: blood pressure level or drug choice
Blood pressure level
Blood pressure is a major risk factor for strokes and it should be treated early and aggressively. Aggressive BP reduction is directly and proportionally associated with decreased stroke incidence (3,8,9), in contrast to CAD incidence, where there is a U-shaped association with the level of BP and the incidence of CAD (10). In the ACCORD study, a mean reduction of SBP to 119.3 mmHg in patients with type 2 diabetes mellitus was associated with a significant (32%) reduction in stroke incidence, but with significantly higher total mortality including a small increase in cardiovascular mortality than mean SBP of 133.5 mmHg (8). Similar findings with the incidence of recurrent strokes were reported by a recent study of 20,330 patients with a non-cardioembolic stroke (9). In this study, different SBP categories were related to recurrent stroke incidence as follows. In patients with very low-normal SBP (SBP <120 mmHg), the stroke incidence was 8%, in those with low-normal SBP (SBP 120 to <130 mmHg) was 7.2%, in those with high-normal SBP (SBP 130 to <140 mmHg) was 6.8%, in those with high SBP (SBP 140-150 mmHg) was 8.7%, and in those with very high SBP (SBP ≥150 mmHg) was 14.1%. This study demonstrated that very low-normal, high, and very high SBP is associated with a higher incidence of recurrent strokes (9). The lowest incidence of recurrent strokes occurred in patients with high-normal SBP of 130 to <140 mmHg. The findings of this study support the recent, more relaxed guidelines for the treatment of hypertension (11). These guidelines recommend a SBP or DBP goal of <150 mmHg and <90 mmHg, respectively for persons ≥60 years old. Treatment to SBP <140 mmHg is also acceptable if well tolerated. For subjects <60 years of age, treatment goals for SBP and DBP are <140 mmHg and <90 mmHg for SBP and DBP, respectively. Besides lowering the BP, early achievement of BP goal is also very important as has been demonstrated by several studies (12). For early and successful BP control two drug combination therapy with either separate or fixed combination can be initiated if the SBP/DBP is 20/10 mmHg over the BP goal.
Drug choice
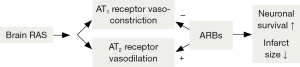
Combinations of diuretics with angiotensin converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs) and beta-blockers (β-blocker) are effective combinations (13). Also, combinations of dihydropyridine calcium channel blockers (CCBs), like amlodipine with ARBs are very effective for BP lowering (14,15). The combination of CCBs with ARBs has been shown to be more effective in stroke prevention than the other drug combinations (16). The brain has its own renin-angiotensin system (RAS), which serves as a local autocrine system to maintain cerebral homeostasis (17). Its significance as a neuroprotector, was not appreciated until recently, when clinical and experimental studies suggested a stroke-protective effect of angiotensin II (Ang II) mediated through its AT2 receptor (Figure 1). The selective blockade of Ang II, AT1 receptor by the ARBs, allows Ang II to stimulate the free AT2. This dual effect of ARBs increases the cerebral blood flow and causes local vasodilation by blocking the vasoconstrictive effects of Ang II through the AT1 receptors and allowing Ang II to stimulate the free AT2 receptors producing additional vasodilation in the local ischemic area of the brain (penumbra) after the onset of stoke. In this respect, the ARBs are superior to ACEIs in stroke protection as has been demonstrated by experimental and clinical studies (17). Medications that stimulate the RAS and the production of Ang II such as diuretics and CCBs are preferable ACE inhibitors and b-blockers for the treatment of hypertensive patients to prevent strokes. The stroke reduction reported in four large clinical trials of older hypertensive patients treated with a diuretic, a CCB, or an ARB-based regimen was impressive. Patients treated with such combinations had a stroke reduction of 29% (18), 36% (19), 40% (20), and 42% (21). In this issue of the journal, Yu et al. present their findings from a “real world” prospective cohort study (22). They included 37,608 hypertensive patients from the “Shanghai Electronic Health Record Management System of Community Residents (SEHRMSCR)”, who were treatment naive for the previous 6 months. Of these patients, 32,682 (86.9%) were started on monotherapy and 4,926 (13.1%) were started on dual combination therapy. Target BP, as expected, was greater and was achieved earlier (6 months) with the dual combination treatment in 60.05% compared with 59.47% with monotherapy. The early reduction of BP was also, associated with a lower incidence of strokes. However, the lower BP achieved with dual combination therapy was lost after 6 months together with the difference in stroke incidence. The reason for this was the significant switch (40.3%) of patients from monotherapy to dual combination therapy during the 42 months of treatment. This resulted in similar BP control in both groups. I am impressed with the percentage of BP goal achieved (80%) and also the drug selection for the treatment of hypertension. In the monotherapy group, CCBs were chosen in 52.10% of cases followed by ARBs in 18.72% of cases. In the dual combination group a CCB-ARB combination was chosen in 39.24% of cases, followed by a CCB-ACEI combination. It appears that Chinese medical practitioners are up to date on current trends for the treatment of hypertension and for the prevention of strokes. This is very important since both ischemic and hemorrhagic strokes are higher in Asian populations than the white populations of European descent (23). The only weakness of this study was the slow achievement of BP goals. Chinese physicians need to be more aggressive in achieving BP goals early to prevent strokes and other target organ damage from hypertension. Overall, this was a very good study demonstrating the benefits of early BP lowering in stroke prevention.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52. [PubMed]
- Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007;25:1105-87. [PubMed]
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903-13. [PubMed]
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29-322. [PubMed]
- Ovbiagele B, Goldstein LB, Higashida RT, et al. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke 2013;44:2361-75. [PubMed]
- Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245-54. [PubMed]
- Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health 2013;1:e259-81. [PubMed]
- ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575-85. [PubMed]
- Ovbiagele B, Diener HC, Yusuf S, et al. Level of systolic blood pressure within the normal range and risk of recurrent stroke. JAMA 2011;306:2137-44. [PubMed]
- Chrysant SG, Chrysant GS. Effectiveness of lowering blood pressure to prevent stroke versus to prevent coronary events. Am J Cardiol 2010;106:825-9. [PubMed]
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. [PubMed]
- Basile JN, Chrysant S. The importance of early antihypertensive efficacy: the role of angiotensin II receptor blocker therapy. J Hum Hypertens 2006;20:169-75. [PubMed]
- Chrysant SG. Using fixed-dose combination therapies to achieve blood pressure goals. Clin Drug Investig 2008;28:713-34. [PubMed]
- Chrysant SG, Melino M, Karki S, et al. The combination of olmesartan medoxomil and amlodipine besylate in controlling high blood pressure: COACH, a randomized, double-blind, placebo-controlled, 8-week factorial efficacy and safety study. Clin Ther 2008;30:587-604. [PubMed]
- Chrysant SG. The role of Angiotensin receptor blocker and calcium channel blocker combination therapy in treating hypertension: focus on recent studies. Am J Cardiovasc Drugs 2010;10:315-20. [PubMed]
- Chrysant SG. Possible pathophysiologic mechanisms supporting the superior stroke protection of angiotensin receptor blockers compared to angiotensin-converting enzyme inhibitors: clinical and experimental evidence. J Hum Hypertens 2005;19:923-31. [PubMed]
- Chrysant SG. The pathophysiologic role of the brain renin-angiotensin system in stroke protection: clinical implications. J Clin Hypertens (Greenwich) 2007;9:454-9. [PubMed]
- PATS Collaborating Group. Post-stroke antihypertensive treatment study. A preliminary result. Chin Med J (Engl) 1995;108:710-7. [PubMed]
- Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997;350:757-64. [PubMed]
- Kjeldsen SE, Dahlöf B, Devereux RB, et al. Effects of losartan on cardiovascular morbidity and mortality in patients with isolated systolic hypertension and left ventricular hypertrophy: a Losartan Intervention for Endpoint Reduction (LIFE) substudy. JAMA 2002;288:1491-8. [PubMed]
- Papademetriou V, Farsang C, Elmfeldt D, et al. Stroke prevention with the angiotensin II type 1-receptor blocker candesartan in elderly patients with isolated systolic hypertension: the Study on Cognition and Prognosis in the Elderly (SCOPE). J Am Coll Cardiol 2004;44:1175-80. [PubMed]
- Yu JM, Kong QY, Shen T, et al. Benefit of initial dual-therapy on stroke prevention in Chinese hypertensive patients: a real world cohort study. J Thorac Dis 2015;7:881-9. [PubMed]
- Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology 2013;81:264-72. [PubMed]


