Primary synovial sarcoma of the lung: can haemothorax be the first manifestation?
Background
Primary pulmonary synovial sarcoma of the lung is exceedingly rare and accounts for 0.5% of primary lung malignancies. We report the case of a 30-year-old man who presented clinically with haemothorax, who was subsequently diagnosed with primary synovial sarcoma of the lung following complete surgical resection of the lesion.
Case report
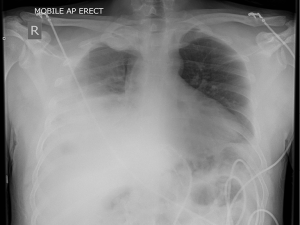
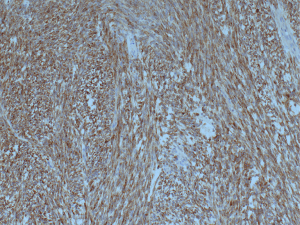
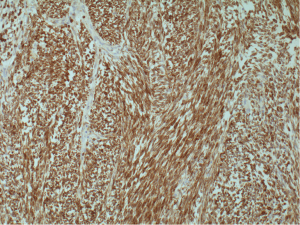
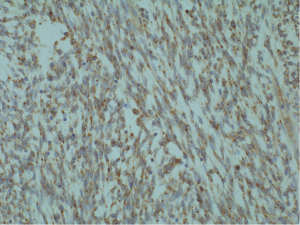
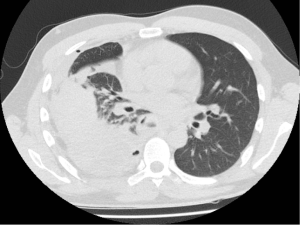
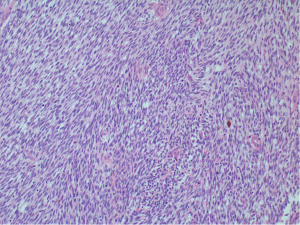
A 30-year-old male presented with 3-week history of fever, cough, and chest pain. He had no medical history of note and was a non-smoker. Clinical examination showed reduced breath sounds and dullness to percussion in the right mid to lower zones. Systemic examination was otherwise unremarkable. Chest radiograph confirmed a large right-sided pleural effusion (Figure 1). A chest drain was inserted which drained blood, revealing that the effusion was in fact a haemothorax. A computer tomography (CT) scan of the chest was performed, which established a complex large effusion obscuring a possible multi-lobulated mass lying posteriorly (Figure 2). A right posterolateral thoracotomy was performed for evacuation of the collection and resection of the right lower lobe, as the lung tissue was necrotic macroscopically. Intra-operative specimens were negative for microbiology. Histological analysis showed pulmonary parenchyma and pleural tissue infiltration by high grade monomorphous spindle cells (Figure 3). High mitotic activity is present and there are diffuse areas of necrosis. Immunohistochemistry of the tumour was positive for EMA (Figure 4) and Bc12 (Figure 5) diffusely and focally for MCK. There was also diffuse dot-like positivity for CD99 (Figure 6). CD34 was negative. Interphase fluorescence in situ hybridisation (FISH) gene rearrangement was positive. These findings are consistent with grade 3 monophasic fibrous synovial sarcoma (pT2b N0 M0 G3).
Post-operatively the course was uneventful and he was discharged on the seventh day and remained well clinically. He has been referred to the oncologist for chemotherapy and further management.
Discussion
Synovial sarcomas are rare mesenchymal tumours accounting for only 8% of soft tissue tumours. They commonly present in soft tissue of extremities in adolescents and young adults, however other sites have been reported including lung, heart, head and neck (1). There are four histological classifications: monophasic fibrous, monophasic epithelial, biphasic (contains both spindle and epithelial cells), and poorly differentiated subtypes.
Primary pulmonary synovial sarcomas are rare and account for approximately 0.5% of lung malignancies. Important differentials of primary pulmonary neoplasm include adenocarcinoma, malignant fibrous histiocytoma, and malignant mesothelioma. Extra-thoracic primary sources should also be excluded as lung metastases from distant synovial sarcomas can also occur (2).
Tumours are often centrally located, with patients frequently presenting with respiratory symptoms including chest pain, cough and haemoptysis. Peripheral tumours are less common. Patients can be asymptomatic initially, present with a pleural effusion when there is invasion of the adjacent pleura (3), or in the case of our patient, with a haemothorax where the tumour has likely infiltrated and bled into the pleural space.
Imaging like chest radiograph and chest CT scans are often carried out as primary investigations, providing information on location and size of lesions, and further information regarding infiltration to adjacent sites. Imaging is non-specific and diagnosis is achieved through histological and immunohistochemistry analysis and can also include cytogenetic testing. Cytogenetic testing is helpful as t(X;18)(p11.2;q11.2) is characteristic of synovial sarcoma, distinguishing it from other soft tissue tumours. There is a range of tests that can be carried out including reverse transcriptase polymerase chain reaction (RT-PCR) to detect gene fusion and product expression, or interphase FISH gene arrangement.
Surgical resection with clear resection margins is the main treatment modality. Prognosis is variable depending on tumour grade; 5-year survival is estimated to be approximately 50%. Adverse prognostic factors include disease stage, increasing age (>20 years old), male gender, large tumour size (>5 cm) and high mitotic activity (>9 mitoses per 10 HPF) (4).
Radiotherapy has no apparent effect on control of local disease or overall survival. Patients may benefit from adjuvant or neoadjuvant chemotherapy, though there is no specific recommended therapy, as studies carried out remain largely inconclusive. This is due to small sample sizes and differing treatments administered in each case (4). Systemic chemotherapy is often administered in palliative cases where surgical resection is not possible (5). In view of high tumour grade and multiple adverse prognostic markers, our patient has been referred for palliative chemotherapy using doxorubicin and ifosfamide, as per local oncology advice.
Given the rapid disease progression and prognostic outcomes, primary pulmonary synovial sarcoma, though rare, should remain an important differential when considering lung malignancies, as complete surgical resection is the mainstay of treatment. Patients may benefit from post-operative adjuvant or neoadjuvant chemotherapy, although evidence remains largely inconclusive till date.
Conclusions
Primary pulmonary synovial sarcoma, though rare, should be considered as one of the differential diagnoses in patients with pulmonary lesions with a variety of clinical presentation as disease progression is rapid, prognostic outcomes are generally unfavourable, and the mainstay of treatment is complete surgical resection, which can only be achieved if diagnosed early.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Dennison S, Weppler E, Giacoppe G. Primary pulmonary synovial sarcoma: a case report and review of current diagnostic and therapeutic standards. Oncologist 2004;9:339-42. [PubMed]
- Aydogdu K, Sahin F, Findik G, et al. Pulmonary synovial sarcoma. Asian Cardiovasc Thorac Ann 2014;22:92-4. [PubMed]
- Roy P, Das A, Sarkar A, et al. A primary synovial sarcoma of lung. N Am J Med Sci 2012;4:241-3. [PubMed]
- Trassard M, Le Doussal V, Hacène K, et al. Prognostic factors in localized primary synovial sarcoma: a multicenter study of 128 adult patients. J Clin Oncol 2001;19:525-34. [PubMed]
- Falkenstern-Ge RF, Kimmich M, Grabner A, et al. Primary pulmonary synovial sarcoma: a rare primary pulmonary tumor. Lung 2014;192:211-4. [PubMed]