Associations between waist circumference, central obesity, and the presence of non-valvular atrial fibrillation patients with heart failure
Highlight box
Key findings
• Waist circumference is related to the presence of heart failure in non-valvular atrial fibrillation (NVAF) patients and can predict the presence of NVAF patients with heart failure.
What is known and what is new?
• Elevated levels of body mass index and waist circumference were associated with an increased risk of atrial fibrillation.
• For NVAF patients with heart failure, we first found waist circumference can predict the incidence of this disease.
What is the implication, and what should change now?
• Our findings may help to improve the treatment and care strategies of NVAF individuals with abdominal obesity.
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, which can lead to heart failure, cardiogenic shock, stroke, and thromboembolic disease and endanger life. Heart failure is a complex syndrome caused by abnormal changes in the structure and function of the heart due to a variety of causes, resulting in dysfunction of ventricular contraction or diastolic function, mainly manifested as dyspnea, decreased exercise tolerance, and fluid retention including pulmonary congestion, systemic congestion and peripheral edema, which is the terminal stage of common clinical heart diseases (1,2). In addition, the occurrence of heart failure following atrial fibrillation (AF) was markedly associated with worse clinical outcomes in terms of morbidity and mortality (3). A study has shown that 37% of people with AF had heart failure. Moreover, people with AF have a nearly 2–5 folds increased risk of heart failure (4). Therefore, determination of the intermediate risk factors is useful for detecting AF in patients with heart failure.
Obesity and the metabolic syndrome associated with obesity are major health problems worldwide (5). The prevalence of obesity, in particular abdominal obesity, predisposes people to a series of cardiovascular risk factors (6,7). Waist circumference (WC) and central obesity (CO) are the indicators most often used to gauge centralized distribution of adipose tissues for assessing individual patients. Compared with general obesity evaluation indicators such as body mass index (BMI), WC or CO have higher value in predicting the risk of cardiovascular diseases (8,9).
Limited recent studies have shown that WC has a significant impact on the prognosis of non-valvular AF (NVAF) patients with heart failure or whether it affects medication adherence (10,11). Therefore, our study aimed to explore the effect of WC on NVAF patients with heart failure in the Chinese population, and to determine the effect of WC on prognosis using data from a cohort of nearly 3,000 patients. We present this article in accordance with the STARD reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-170/rc).
Methods
Participants
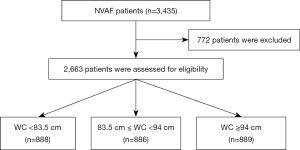
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This is a retrospective cohort study based on the database of Shang et al. (12) which was conducted from January 2015 to December 2017 and included 3,435 NVAF patients at the First Affiliated Hospital of Xinjiang Medical University. After excluding 772 patients who did not answer the information about their WC, 2,663 patients were enrolled in our study. In the original article, the authors reported that the study had been approved by the Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University and that informed consent has been provided by the participants.
Data
In this secondary analysis, WC and CO were used as the exposure variables and NVAF with heart failure was used as the outcome variable. The 2,663 patients were divided into three groups stratified by WC into triples: WC <83.5 cm, 83.5 cm ≤ WC <94 cm, WC ≥94 cm. We defined CO as the dichotomous variable based on the WC measurement standard of the World Health Organization (WHO), clinical action thresholds of the third National Health and Nutrition Examination Survey, and the previous research, with WC ≥94 cm for men and WC ≥80 cm for women being classified as CO (13-15). In this study, continuous variables included age, height, WC, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose (FBG), homocysteine (HCY), triglyceride (TG), total cholesterol (TC), and low-density lipoprotein cholesterol (LDLC). Categorical variables included sex, education, smoking, drink, CO, complications such as heart failure, hypertension, diabetes mellitus (DM), stroke, vascular disease, and plaque.
Statistical analysis
Data was analyzed with the use of the statistical package R version 3.4.3 (The R Foundation, Vienna, Austria; http://www.r-project.org). The continuous variables were indicated by mean and standard deviation. The classification variables were expressed as percentages. Analysis of variance (ANOVA) was used to analyze the relationship between continuous variables and categorical variables. Kruskal-Wallis test was used to analyze the relationship among categorical variables. The baseline characteristic table was divided into three groups according to the tertiles of WC. The P value was calculated by parametric and nonparametric tests. Based on the significant variables (P≤0.05) in univariate analysis, multiple regressions and the subgroup analysis were conducted in order to obtain the result of the trend test for the variables. We created three models: Model 1 adjusted for none; Model 2 adjusted for age and sex; Model 3 adjusted for age, sex, education, smoking, alcohol consumption, height, BMI, SBP, DBP, FBG, HCY, TG, TC, and LDLC, and complications such as heart failure, hypertension, DM, stroke, vascular disease, and plaque. To identify indicators of NVAF patients with heart failure, we performed receiver operating characteristic (ROC) curve analysis. Sensitivity and specificity were then calculated for each of the arithmetic indicators for NVAF patients with heart failure. A P value less than 0.05 indicated that the difference was statistically significant.
Sensitivity analysis
To verify whether the results were reliable, we conducted the following sensitivity analysis: (I) conversion of continuous variables into categorical variables for analysis; (II) univariate analysis and the multiple regressions were conducted to investigate the changes of core results; (III) subgroup analysis was conducted to observe the influence of other factors on the effect of WC and CO on NVAF with heart failure.
Results
Baseline characteristics
After excluding 772 patients who were lacking information about their WC, 2,663 NVAF patients were enrolled in our study (Figure 1). Table 1 shows the distribution of clinical characteristics for different WC groups. There was no significant difference in the general conditions (education, smoking, alcohol consumption) and the complication of stroke between different groups. In the group of WC ≥94 cm, patients with NVAF had the highest probability of the complication of heart failure. In all groups, the probability of complications (hypertension, DM), the clinical data (BMI, systolic, diastolic, FBG, HCY, TG, TC, LDLC), and the average age of patients increased alongside the increasing level of WC.
Table 1
| Variable | WC (cm) | P value | P value* | ||
|---|---|---|---|---|---|
| <83.5 (n=888) | ≥83.5, <94 (n=886) | ≥94 (n=889) | |||
| Heart failure, n (%) | 19 (2.1) | 55 (6.2) | 252 (28.3) | <0.001 | – |
| Age, year, mean ± SD | 62.5±9.9 | 63.2±9.9 | 64.2±9.0 | <0.001 | <0.001 |
| Gender, n (%) | |||||
| Male | 292 (32.9) | 358 (40.4) | 389 (43.8) | <0.001 | – |
| Female | 596 (67.1) | 528 (59.6) | 500 (56.2) | <0.001 | – |
| Education level, n (%) | 0.05 | – | |||
| Primary school and below | 470 (52.9) | 480 (54.2) | 519 (58.4) | ||
| Middle school | 250 (28.2) | 266 (30.0) | 248 (27.9) | ||
| High school or higher | 168 (8.9) | 140 (15.8) | 122 (13.7) | ||
| Current smoking, n (%) | 158 (17.8) | 163 (18.4) | 137 (15.4) | 0.21 | – |
| Current drinking, n (%) | 764 (86.0) | 747 (84.3) | 743 (83.6) | 0.33 | – |
| Height, cm, mean ± SD | 160.7±10.4 | 162.3±9.1 | 163.1±8.5 | <0.001 | <0.001 |
| SBP, mmHg, mean ± SD | 137.8±19.5 | 143.4±21.0 | 147.7±22.1 | <0.001 | <0.001 |
| DBP, mmHg, mean ± SD | 83.2±11.3 | 86.0±12.3 | 86.3±12.6 | <0.001 | <0.001 |
| FBG, mmol/L, mean ± SD | 5.8±1.7 | 6.1±2.1 | 6.3±2.1 | <0.001 | <0.001 |
| TG, mmol/L, mean ± SD | 1.5±0.9 | 1.7±1.1 | 2.0±1.3 | <0.001 | <0.001 |
| TC, mmol/L, mean ± SD | 4.9±1.1 | 5.0±1.2 | 5.1±1.2 | 0.005 | 0.002 |
| LDL-C, mmol/L, mean ± SD | 2.9±1.0 | 3.0±0.9 | 3.1±1.0 | <0.001 | <0.001 |
| HCY, mmol/L, mean ± SD | 12.6±8.8 | 16.0±10.7 | 16.3±8.9 | <0.001 | <0.001 |
| Plaque, n (%) | 411 (46.3) | 475 (53.6) | 467 (52.5) | 0.004 | – |
| Hypertension, n (%) | 527 (59.3) | 584 (65.9) | 637 (71.7) | <0.001 | – |
| DM, n (%) | 173 (19.5) | 198 (22.3) | 230 (25.9) | 0.005 | – |
| Stroke, n (%) | 101 (11.4) | 116 (13.1) | 106 (11.9) | 0.52 | – |
| Vascular disease, n (%) | 565 (63.6) | 528 (59.6) | 517 (58.2) | 0.05 | – |
*, calculated by Kruskal-Wallis H test. WC, waist circumference; SD, standard deviation; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; TG, triglyceride; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HCY, homocysteine; DM, diabetes mellitus.
The relationship of WC and CO on NVAF patients with heart failure
According to the results of the univariate analysis in Table 2, the following factors had significant statistical differences with heart failure: age, sex, height, WC, CO, BMI, SBP, FBG, HCY, TG, LDLC, hypertension, DM, stroke, vascular disease, and plaque (P<0.05). However, there was no correlation between NVAF patients with heart failure and education, smoking, alcohol consumption, DBP, TC (P>0.05). In the analysis using baseline clinical characteristics (Table 1) and the univariate analysis (Table 2), we found a clear positive correlation between both WC and CO and NVAF with heart failure. According to the WHO’s criteria, we classified WC into a dichotomous variable (≥94 cm for men and ≥80 cm for women) which we called CO (16). In the non-adjusted model in Table 3, the disease risk of NVAF with heart failure increased by 10% with an increase of WC of 1 cm. Similarly, patients with CO had a 2.8-fold increased risk of disease progression compared with those without CO. We observed similar results in the minimally adjusted model and the fully adjusted model. Therefore, WC and CO were independent predictors of NVAF with heart failure respectively. As shown in Table 3, each body mass index (BMI) category had a strong correlation with the presence of NVAF patients with heart failure in the non-adjusted model and the minimally adjusted model, but there was no significant association in the fully adjusted model, indicating that BMI was not an independent predictor of the presence of NVAF patients with heart failure.
Table 2
| Variable | With heart failure | OR | 95% CI | P value |
|---|---|---|---|---|
| Age, year, mean ± SD | 63.3±9.6 | 1.0 | 1.0, 1.0 | <0.001 |
| Male, n (%) | 1,039 (39.0) | 1.0 | 1.0, 1.0 | <0.001 |
| Female, n (%) | 1,624 (61.0) | 0.6 | 0.5, 0.7 | <0.001 |
| Education level, n (%) | ||||
| Primary school and below | 1,469 (55.2) | 1.0 | 1.0, 1.0 | <0.001 |
| Middle school | 764 (28.7) | 0.9 | 0.7, 1.2 | 0.64 |
| High school or higher | 430 (16.1) | 0.8 | 0.6, 1.2 | 0.30 |
| Current smoking, n (%) | 458 (17.2) | 1.0 | 0.8, 1.4 | 0.88 |
| Current drinking, n (%) | 2,254 (84.6) | 0.8 | 0.6, 1.1 | 0.25 |
| Height, cm, mean ± SD | 162.0±9.4 | 1.0 | 1.0, 1.0 | 0.002 |
| WC, cm, mean ± SD | 88.5±11.7 | 1.1 | 1.1, 1.1 | <0.001 |
| CO, n (%) | 1,530 (57.5) | 3.8 | 2.8, 5.0 | <0.001 |
| SBP, mmHg, mean ± SD | 142.9±21.3 | 1.0 | 1.0, 1.0 | <0.001 |
| DBP, mmHg, mean ± SD | 85.2±12.2 | 1.0 | 1.0, 1.0 | 0.13 |
| FBG, mmol/L, mean ± SD | 6.1±2.0 | 1.1 | 1.0, 1.1 | 0.04 |
| HCY, mmol/L, mean ± SD | 15.0±9.6 | 1.0 | 1.0, 1.0 | 0.002 |
| TG, mmol/L, mean ± SD | 1.7±1.1 | 1.1 | 1.0, 1.2 | 0.01 |
| TC, mmol/L, mean ± SD | 5.0±1.2 | 1.1 | 1.0, 1.2 | 0.08 |
| LDLC, mmol/L, mean ± SD | 3.0±1.0 | 1.2 | 1.0, 1.3 | 0.02 |
| Plaque, n (%) | 1,353 (50.8) | 1.9 | 1.5, 2.4 | <0.001 |
| Hypertension, n (%) | 1,748 (65.6) | 1.5 | 1.1, 1.9 | 0.003 |
| DM, n (%) | 601 (22.6) | 1.3 | 1.0, 1.7 | 0.03 |
| Stroke, n (%) | 323 (12.1) | 1.7 | 1.2, 2.3 | <0.001 |
| Vascular disease, n (%) | 1,610 (60.5) | 0.7 | 0.6, 0.9 | 0.005 |
NVAF, non-valvular atrial fibrillation; OR, odds ratio; CI, confidence interval; SD, standard deviation; WC, waist circumference; CO, central obesity; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; HCY, homocysteine; TG, triglyceride; TC, total cholesterol; LDLC, low-density lipoprotein cholesterol; DM, diabetes mellitus.
Table 3
| Exposure | Non-adjusted model OR (95% CI) |
Minimally-adjusted model OR (95% CI) |
Fully-adjusted model OR (95% CI) |
P value |
|---|---|---|---|---|
| WC, cm | 1.1 (1.1, 1.1) | 1.1 (1.1, 1.1) | 1.1 (1.1, 1.1) | <0.001 |
| <83.5 | Ref | Ref | Ref | |
| ≥83.5, <94 | 3.0 (1.8, 5.1) | 2.9 (1.7, 4.9) | 2.6 (1.5, 4.6) | <0.001 |
| ≥94 | 18.1 (11.2, 29.2) | 17.2 (10.6, 27.7) | 15.7 (9.3, 26.6) | <0.001 |
| CO | 3.8 (2.8, 5.0) | 6.0 (4.4, 8.3) | 6.0 (4.2, 8.4) | <0.001 |
Non-adjusted model adjusted for none; minimally-adjusted model adjusted for age and sex; fully-adjusted model adjusted for age, sex, education, smoking, drink, height, systolic, diastolic, FBG, HCY, TG, TC, LDLC and complications such as heart failure, hypertension, DM, stroke, vascular disease, and plaque. WC, waist circumference; CO, central obesity; NVAF, non-valvular atrial fibrillation; OR, odds ratio; CI, confidence interval; FBG, fasting blood glucose; HCY, homocysteine; TG, triglyceride; TC, total cholesterol; LDLC, low-density lipoprotein cholesterol; DM, diabetes mellitus.
The results of the sensitivity analyses
The subgroup analysis displayed in Table 4 was conducted to explore the relationship between WC and NVAF with heart failure in each stratification of age, sex, height, SBP, DBP, TG, TC, and LDLC. Each stratification adjusted for all the factors (age, height, SBP, DBP, FBG, HCY, TG, TC, LDLC, sex, education, smoking, alcohol consumption, CO, hypertension, DM, stroke, vascular disease, and plaque) except the stratification factor itself. We found that the value of the odds ratio (OR) was above 1, indicating that the relationship of WC and NVAF with heart failure within each stratification of the factors above was consistent and all the covariates were risk factors. Furthermore, an interaction between age, sex, and WC were observed in our study. According to the interaction P value, the effect of WC on NVAF patients with heart failure was significantly different according to age and sex (P<0.05). Our results indicated that WC was positively associated with NVAF patients with heart failure in male [OR =1.08, 95% confidence interval (CI): 1.06–1.1].
Table 4
| Variable | N | OR | 95% CI | Interaction P value |
|---|---|---|---|---|
| Age (year) | <0.001 | |||
| 40–58 | 804 | 1.13 | 1.10, 1.16 | |
| 59–67 | 971 | 1.14 | 1.11, 1.17 | |
| 68–96 | 888 | 1.06 | 1.04, 1.07 | |
| Sex | 0.01 | |||
| Male | 1,039 | 1.08 | 1.06, 1.10 | |
| Female | 1,624 | 1.11 | 1.09, 1.13 | |
| Height (cm) | 0.21 | |||
| 150–158 | 884 | 1.09 | 1.07, 1.12 | |
| 158.1–164.9 | 743 | 1.12 | 1.09, 1.15 | |
| 165–189 | 1,036 | 1.10 | 1.08, 1.11 | |
| SBP (mmHg) | 0.19 | |||
| 87–131 | 852 | 1.10 | 1.08, 1.13 | |
| 132–149 | 829 | 1.11 | 1.09, 1.14 | |
| 150–238 | 977 | 1.08 | 1.06, 1.10 | |
| DBP (mmHg) | 0.55 | |||
| 43–79 | 677 | 1.10 | 1.07, 1.13 | |
| 80–89 | 962 | 1.11 | 1.08, 1.13 | |
| 90–159 | 1,019 | 1.09 | 1.07, 1.11 | |
| TG (mg/dL) | 0.48 | |||
| 0.09–1.16 | 877 | 1.09 | 1.06, 1.11 | |
| 1.17–1.79 | 885 | 1.09 | 1.07, 1.12 | |
| 1.8–11.1 | 890 | 1.11 | 1.08, 1.13 | |
| TC (mg/dL) | 0.43 | |||
| 0.27–4.49 | 872 | 1.09 | 1.07, 1.12 | |
| 4.5–5.44 | 890 | 1.11 | 1.09, 1.13 | |
| 5.45–9.31 | 886 | 1.09 | 1.07, 1.11 | |
| LDLC (mg/dL) | 0.18 | |||
| 0.06–2.49 | 872 | 1.09 | 1.08, 1.13 | |
| 2.5–3.29 | 880 | 1.11 | 1.09, 1.14 | |
| 3.3–7.1 | 894 | 1.08 | 1.06, 1.10 |
NVAF, non-valvular atrial fibrillation; SBP, systolic blood pressure; DBP, diastolic blood pressure; TG, triglyceride; TC, total cholesterol; LDLC, low-density lipoprotein cholesterol; OR, odds ratio; CI, confidence interval.
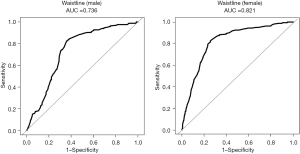
The predictive value of WC and CO for the disease risk of NVAF with heart failure
To determine the most predictive and minimalistic model, we plotted ROC curves for the disease risk of NVAF with heart failure (Figure 2, Table 5). Our results observed that WC had higher predictive power than CO (0.638) and BMI (0.619), with an area under the ROC curve (AUC) of 0.785 (P<0.0001). Compared with CO and BMI, WC in general had better specificity (0.6688:0.4591), sensitivity (0.8466:0.8160) and accuracy (0.6906:0.5028). Furthermore, the proposed cut-off value of WC for predicting NVAF with heart failure is 91.85 cm for males and 93.15 cm for females. The diagnostic value of WC for NVAF with heart failure was higher for females than it was for males and its AUC is larger (0.821:0.736) (Figure 3).
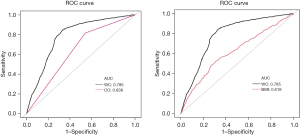
Table 5
| Variable | WC | CO |
|---|---|---|
| AUC | 0.785 | 0.638 |
| Specificity | 0.6688 | 0.4591 |
| Sensitivity | 0.8466 | 0.8160 |
| Accuracy | 0.6906 | 0.5028 |
WC, waist circumference; CO, central obesity; NVAF, non-valvular atrial fibrillation; AUC, area under the curve.
Discussion
This study is the first to investigate the influence of WC and CO on NVAF patients with heart failure. Our study is based on a secondary analysis of 2,663 patients. The identified risk factors of NVAF with heart failure were sex, height, WC, CO, FBG, HCY, TG, LDLC, hypertension, DM, stroke, vascular disease, and plaque. Then, a binary logistic regression model indicated that the occurrence of NVAF patients with heart failure increased 10% with WC increasing 1 cm and had a 2.8-fold increased risk with CO compared to those without. Furthermore, the predictive value (AUC), specificity, sensitivity and accuracy of WC for the disease risk of NVAF with heart failure were higher than CO. Our proposed cut-off value of WC for is 91.85 cm for males and 93.15 cm for females. The diagnostic value of WC for NVAF with heart failure was higher for females than it was for males.
Obesity is a multifactorial disease, which is caused by the imbalance between energy intake (EI) and total energy expenditure (TEE) (16,17). This imbalance will lead to the accumulation of excess fat in the body and is related to changes in many metabolic pathways (18,19). A previous study has shown that the 1-year mortality risk of AF patients was negatively related to high BMI, and was directly related to the presence of chronic kidney disease, carotid stenosis, and chronic heart failure in the cohort of AF patients (20). In underweight and normal-weight Asian populations, BMI variability, particularly weight gain, has been associated with an increased risk of new-onset AF and myocardial infarction (21). Obesity, no matter whether defined by BMI or WC, is significantly associated with AF (22). WC and CO have a stronger correlation with the prevalence of cardiovascular disease because they can identify individuals with low body weight but increased ectopic fat accumulation (19,23-25). Abdominal obesity has been highlighted as an important, potentially modifiable risk factor for AF in non-obese Asian populations (26). The American Diabetes Association (ADA) recommends that WC be measured as an alternative indicator of abdominal fat, because it is related to the risk of heart metabolism and emphasizes the difficulty of accurately measuring abdominal fat (27). They quoted WC >102 cm for males and WC >88 cm for females to evaluate the increased risk of heart metabolic disease (28). In addition, WC is associated with congestive heart failure and all-cause mortality independently in patients with type 2 diabetes (16).
Our research has several benefits. First, this is the first time that WC, as an indicator of abdominal obesity, has been utilized to predict the incidence of NVAF with heart failure. Further, our study indicated that the cut-off value of WC for predicting -presence of NVAF with heart failure should be 91.85 cm for males and 93.15 cm for females. However, the validity of this research may be limited to the ethnic group being studied. Therefore, more investigations should be conducted to probe the obesity risk in this category of patients. Our findings indicated that clinical and public health interventions should aim to maintain optimal WC level, which might be an efficient approach to prevent the development of AF.
Our study has several limitations. Firstly, the cases included were Chinese patients with NVAF and thus it has certain geographical and ethnic limitations. Secondly, due to our inclusion standards, the cases did not include patients who had a history of carotid endarterectomy, carotid artery stent implantation or had experienced significant carotid malformation. Thirdly, because this study is a secondary analysis, we can only adjust the original variables in the database.
Conclusions
Our research revealed that WC is related to the presence of heart failure in the patients with NYAF and can be used to predict the presence of NAVF patients with heart failure. Our findings may help to improve the treatment and care strategies of patients with heart failure and abdominal obesity.
Acknowledgments
This manuscript was written on behalf of AME Cardiology Collaborative Group. The authors express their gratitude to the Departments that provided the funding for this study, and the medical personnel of The Affiliated Hospital of Guizhou Medical University.
Funding: This work was funded by
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-170/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-170/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-24-170/coif). C.E. received honoraria for lectures from AstraZeneca, Novartis, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Pfizer, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tanai E, Frantz S. Pathophysiology of Heart Failure. Compr Physiol 2015;6:187-214. [Crossref] [PubMed]
- Baman JR, Passman RS. Atrial Fibrillation. JAMA 2021;325:2218. [Crossref] [PubMed]
- Taniguchi N, Miyasaka Y, Suwa Y, et al. Heart Failure in Atrial Fibrillation- An Update on Clinical and Echocardiographic Implications. Circ J 2020;84:1212-7. [Crossref] [PubMed]
- Carlisle MA, Fudim M, DeVore AD, et al. Heart Failure and Atrial Fibrillation, Like Fire and Fury. JACC Heart Fail 2019;7:447-56. [Crossref] [PubMed]
- Vecchié A, Dallegri F, Carbone F, et al. Obesity phenotypes and their paradoxical association with cardiovascular diseases. Eur J Intern Med 2018;48:6-17. [Crossref] [PubMed]
- Grundy SM, Neeland IJ, Turer AT, et al. Waist circumference as measure of abdominal fat compartments. J Obes 2013;2013:454285. [Crossref] [PubMed]
- Elagizi A, Kachur S, Carbone S, et al. A Review of Obesity, Physical Activity, and Cardiovascular Disease. Curr Obes Rep 2020;9:571-81. [Crossref] [PubMed]
- Britton KA, Massaro JM, Murabito JM, et al. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol 2013;62:921-5. [Crossref] [PubMed]
- Lam BC, Koh GC, Chen C, et al. Comparison of Body Mass Index (BMI), Body Adiposity Index (BAI), Waist Circumference (WC), Waist-To-Hip Ratio (WHR) and Waist-To-Height Ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS One 2015;10:e0122985. [Crossref] [PubMed]
- Wang W, Tan JS, Wang J, et al. Genetically predicted waist circumference and risk of atrial fibrillation. Chin Med J (Engl) 2024;137:82-6. [Crossref] [PubMed]
- Poorthuis MHF, Sherliker P, de Borst GJ, et al. Joint Associations Between Body Mass Index and Waist Circumference With Atrial Fibrillation in Men and Women. J Am Heart Assoc 2021;10:e019025. [Crossref] [PubMed]
- Shang L, Zhao Y, Shao M, et al. The association of CHA2DS2-VASc score and carotid plaque in patients with non-valvular atrial fibrillation. PLoS One 2019;14:e0210945. [Crossref] [PubMed]
- Han TS, van Leer EM, Seidell JC, et al. Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ 1995;311:1401-5. [Crossref] [PubMed]
- Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ 1995;311:158-61. [Crossref] [PubMed]
- Zhu S, Wang Z, Heshka S, et al. Waist circumference and obesity-associated risk factors among whites in the third National Health and Nutrition Examination Survey: clinical action thresholds. Am J Clin Nutr 2002;76:743-9. [Crossref] [PubMed]
- German CA, Laughey B, Bertoni AG, et al. Associations between BMI, waist circumference, central obesity and outcomes in type II diabetes mellitus: The ACCORD Trial. J Diabetes Complications 2020;34:107499. [Crossref] [PubMed]
- Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res 2017;122:1-7. [Crossref] [PubMed]
- Alfredo Martínez J. Perspectives on personalized nutrition for obesity. J Nutrigenet Nutrigenomics 2014;7:I-III. [Crossref] [PubMed]
- Xue R, Li Q, Geng Y, et al. Abdominal obesity and risk of CVD: a dose-response meta-analysis of thirty-one prospective studies. Br J Nutr 2021;126:1420-30. [Crossref] [PubMed]
- Rodríguez-Reyes H, Lara-Vaca S, Ochoa-Guzmán A, et al. Obesity Paradox and 12 Month Outcome in Patients with Atrial Fibrillation. Arch Med Res 2021;52:233-9. [Crossref] [PubMed]
- Lim YM, Yang PS, Jang E, et al. Body Mass Index Variability and Long-term Risk of New-Onset Atrial Fibrillation in the General Population: A Korean Nationwide Cohort Study. Mayo Clin Proc 2019;94:225-35. [Crossref] [PubMed]
- Zhao M, Song L, Zhao Q, et al. Elevated levels of body mass index and waist circumference, but not high variability, are associated with an increased risk of atrial fibrillation. BMC Med 2022;20:215. [Crossref] [PubMed]
- Lee CM, Huxley RR, Wildman RP, et al. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 2008;61:646-53. [Crossref] [PubMed]
- Menke A, Muntner P, Wildman RP, et al. Measures of adiposity and cardiovascular disease risk factors. Obesity (Silver Spring) 2007;15:785-95. [Crossref] [PubMed]
- Brenner DR, Tepylo K, Eny KM, et al. Comparison of body mass index and waist circumference as predictors of cardiometabolic health in a population of young Canadian adults. Diabetol Metab Syndr 2010;2:28. [Crossref] [PubMed]
- Baek YS, Yang PS, Kim TH, et al. Associations of Abdominal Obesity and New-Onset Atrial Fibrillation in the General Population. J Am Heart Assoc 2017;6:e004705. [Crossref] [PubMed]
- Klein S, Allison DB, Heymsfield SB, et al. Waist Circumference and Cardiometabolic Risk: a Consensus Statement from Shaping America's Health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Obesity (Silver Spring) 2007;15:1061-7. [Crossref] [PubMed]
- National Institutes of Health, National Heart, Lung, and Blood Institute, NHLBI Obesity Education Initiative, North American Association for the Study of Obesity. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. NIH Publication 2000;00-4084.