
Effect of particulate matter on continuous positive airway pressure adherence in obstructive sleep apnea patients
Highlight box
Key findings
• There was no effect of particulate matter on continuous positive airway pressure (CPAP) adherence in obstructive sleep apnea (OSA) patients.
What is known and what is new?
• Sleep quality could be affected by particulate matter with a diameter of less than 10 microns (PM10) and particulate matter with a diameter of less than 2.5 microns (PM2.5).
• Air pollution especially for PM10 and PM2.5 were not associated with low CPAP adherence in OSA patients.
What is the implication, and what should change now?
• Air purifiers should be still suggested for CPAP users during high air pollution periods.
Introduction
Obstructive sleep apnea (OSA) is a prevalent sleep disorder that impacts 3–9% of the general population and it has been identified as a risk factor for a range of health conditions, including hypertension, cardiovascular disease, neurological disorders, and psychiatric illnesses (1). The utilization of continuous positive airway pressure (CPAP) is a highly efficacious approach for treating OSA and is widely regarded as the preeminent therapeutic intervention for this condition. However, the adherence of patients to this treatment is crucial for its overall effectiveness (2-4). The efficacy of CPAP therapy is closely linked to adherence to treatment, rendering it a highly effective intervention. Nevertheless, ensuring adherence to CPAP therapy continues to pose difficulties. The CPAP therapy is recommended to be administered throughout the entirety of a patient’s sleep cycle. However, it has been observed that this protocol is only adhered to by a minority of subjects in practical settings.
Numerous studies have demonstrated that a variety of factors including subjective sleep-related symptoms, the OSA severity, awareness of CPAP’s effects and side effects, and discomfort affect adherence to CPAP therapy (5-7). Our recent study has also shown that low CPAP adherence in elderly OSA patients are caused by females gender, personal life issues and adverse attitudes towards treatment, and health issues (8).
The issue of air pollution holds significant global importance. The majority of the global population resides in regions where the concentrations of air pollutants surpass the thresholds established by the World Health Organization (WHO) guidelines, with a percentage exceeding 90%. Air pollution is a major problem in Chiang Mai, Thailand. During pre-summer and summer seasons (January–April), air pollutant levels especially for particulate matter with a diameter of less than 2.5 microns (PM2.5) usually exceed the WHO safety threshold. For over a decade, the correlation between air pollution and adverse health consequences in this region has been acknowledged especially in subjects with cardiopulmonary diseases (9-14).
Sleep quality could be affected by air pollution, especially for particulate matter with a diameter of less than 10 microns (PM10) and PM2.5 (15-20). Previous studies showed that the particular matter (PM) was associated with an increase in apnea-hypopnea index (AHI) both without and even while using CPAP (15,16,19). Moreover, significant changes in sleep parameters including oxygen desaturation index, and total sleep time with peripheral capillary oxygen saturation (SpO2) lower than 90% in chronic obstructive pulmonary disease (COPD) patients with OSA were also found (20). Currently, no direct study demonstrates the relationship and impact of air pollution especially PM10 and PM2.5 on CPAP adherence. Therefore, we aimed to study the association between PM10, PM2.5, and low CPAP adherence in subjects with OSA. We present this article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1507/rc).
Methods
Design and study participants
We conducted a time-series study from August 2016 to May 2022 in Chiang Mai, Thailand. The data from 2,686 visits of CPAP compliance records from 839 OSA patients’ electronic medical records at the Sleep Disorders Center, Center of Medical Excellence, Chiang Mai University, Chiang Mai, Thailand were reviewed. The evaluation of compliance with CPAP therapy was consistently conducted through the objective analysis of the electronic data recording of CPAP devices. The level of adherence was determined utilizing the provided data. Low CPAP adherence was defined as using CPAP for less than 240 minutes per night or less than 70% of nights (i.e., <5 nights/week) (21). We used an average data of CPAP adherence in the previous month. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University [Institutional Review Board (IRB) approval number: MED-2565-09282, date of approval 18 November 2022]. Individual consent for this retrospective analysis was waived.
Measurements of air pollutants
The measurements of air quality were recorded by Air Quality and Noise Management, Division Pollution Control Department, Thailand, and the sampling station is located at the center of Muang District, Chiang Mai Province, Thailand (22). Monthly average concentrations for PM10, PM2.5, sulfur dioxide (SO2), nitrogen dioxide (NO2), and ozone (O3) were recorded. However, the monthly average concentration of carbon monoxide (CO) has not been available in Chiang Mai station since July 2016. The meteorological data including temperature, atmospheric pressure, rain, relative humidity, and wind speed were obtained from the Northern Meteorology Center, Chiang Mai province on an average monthly basis (23). We retrieved data from August 2016 to May 2022 in parallel with CPAP adherence data.
Statistical analysis
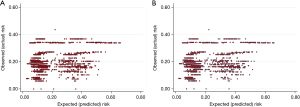
Results for continuous data were shown as mean ± standard deviation (SD) or median and interquartile range (IQR). The categorical data were expressed as absolute frequencies and percentages. The correlation coefficients among the air pollutants were calculated using Pearson’s correlation (r). The correlation between the monthly average of PM10 and PM2.5 and the low CPAP adherence was analyzed using generalized linear mixed model (GLMM) after adjustment for other ambient pollutants including SO2, NO2, O3, meteorological parameters including temperature, atmospheric pressure, rain, relative humidity, and wind speed, age, sex, personal life issues, and adverse attitudes towards CPAP treatment, and health conditions. The correlation between the monthly average concentrations of PM10 and PM2.5 and the rate of low CPAP adherence was examined for the lag of 0 months. The month of an increase in monthly average PM10 and PM2.5 were defined as lag time 0 (lag0). Results were displayed as adjusted risk ratios (RRs) with 95% confidence intervals (CIs). Model calibration was evaluated using a calibration plot between observed (actual) risk and expected (predicted) risk. Statistical significance was accepted at a P value less than 0.05. We used StataCorp version 16.1, College Station, TX, USA) for statistical analysis.
Results
There was a total of 2,686 visits from 839 OSA patients from August 2016 to May 2022. The patients’ characteristics are shown in Table 1. The mean age was 56.6±14.7 years old, with 296 (35.3%) males. More data are shown in Table 1.
Table 1
| Characteristics | Values |
|---|---|
| Age (years) | 56.6±14.7 |
| Sex (male) | 296 (35.3) |
| BMI (kg/m2) | 27.8±5.6 |
| Neck circumference (inch) | 15.5±2.1 |
| Waist circumference (inch) | 39.3±8.9 |
| Comorbidities | |
| Coronary artery disease | 7 (0.8) |
| COPD | 6 (0.7) |
| Diabetes mellitus | 31 (3.7) |
| Hypertension | 80 (9.5) |
| EDS defined by ESS | 485 (57.8) |
| AHI total | 71.1 (53.9, 90.3) |
| AHI REM | 0.0 (0.0, 53.8) |
| AHI non-REM | 72.8 (53.9, 92.1) |
Values are presented as mean ± SD, n (%), or median (IQR). OSA, obstructive sleep apnea; BMI, body mass index; COPD, chronic obstructive pulmonary disease; EDS, excessive daytime sleepiness; ESS, Epworth Sleepiness Scale; AHI, apnea-hypopnea index; REM, rapid eye movement; SD, standard deviation; IQR, interquartile range.
The monthly average PM10 and PM2.5 and number of low CPAP adherence throughout the study period is shown in Figure 1. PM10 and PM2.5 levels increased during dry season (January–April) of every year.
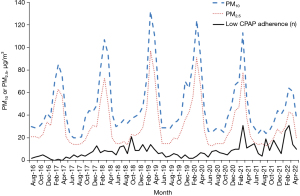
The correlation coefficients among the air pollutants are shown in Table 2. There was a high correlation between PM10 and PM2.5 with r=0.996.
Table 2
| Pollutants | PM10 (µg/m3) | PM2.5 (µg/m3) | O3 (ppb) | NO2 (ppb) | SO2 (ppb) |
|---|---|---|---|---|---|
| PM10 (µg/m3) | 1.000 | ||||
| PM2.5 (µg/m3) | 0.996 | 1.000 | |||
| O3 (ppb) | 0.836 | 0.818 | 1.000 | ||
| NO2 (ppb) | 0.658 | 0.663 | 0.529 | 1.000 | |
| SO2 (ppb) | 0.246 | 0.246 | 0.210 | 0.138 | 1.000 |
PM10, particulate matters with diameter of less than 10 microns; PM2.5, particulate matters with diameter of less than 2.5 microns; O3, ozone; NO2, nitrogen dioxide; SO2, sulfur dioxide.
The effect of every 10 µg/m3 increase in PM10 and PM2.5 on low CPAP adherence was demonstrated in Table 3. There was no effect of an increase in PM10 and PM2.5 on low CPAP adherence after adjustment for confounding factors including SO2, NO2, and O3, temperature, atmospheric pressure, rain, relative humidity, and wind speed, age, sex, personal life issues and adverse attitudes towards CPAP treatment, and health conditions (adjusted RR of 0.97; 95% CI: 0.87, 1.09; P value =0.624 and 0.93; 95% CI: 0.81, 1.08; P value =0.350 for PM10 and PM2.5, respectively). We also found no effect of an increase in PM10 and PM2.5 on low CPAP adherence in stratified analysis for sex (male and female) and age group (<60 and ≥60 years).
Table 3
| Pollutions | Adjusted risk ratios (95% CI)† | P value |
|---|---|---|
| Total subjects | ||
| PM10 (µg/m3) | 0.97 (0.87, 1.09) | 0.624 |
| PM2.5 (µg/m3) | 0.93 (0.81, 1.08) | 0.350 |
| Male | ||
| PM10 (µg/m3) | 0.95 (0.20, 1.12) | 0.521 |
| PM2.5 (µg/m3) | 0.91 (0.73, 1.12) | 0.383 |
| Female | ||
| PM10 (µg/m3) | 0.99 (0.86, 1.15) | 0.899 |
| PM2.5 (µg/m3) | 0.95 (0.79, 1.14) | 0.599 |
| Age <60 years | ||
| PM10 (µg/m3) | 0.89 (0.75, 1.07) | 0.227 |
| PM2.5 (µg/m3) | 0.84 (0.67, 1.06) | 0.135 |
| Age ≥60 years | ||
| PM10 (µg/m3) | 1.03 (0.89, 1.19) | 0.693 |
| PM2.5 (µg/m3) | 1.00 (0.84, 1.20) | 0.983 |
†, adjusted for age, sex, other pollutants including SO2, NO2, and O3, meteorological parameters including temperature, atmospheric pressure, rain, relative humidity, and wind speed, age, sex, personal life issues and adverse attitudes, and health-related problems. PM10, particulate matter with a diameter of less than 10 microns; PM2.5, particulate matter with a diameter of less than 2.5 microns; CPAP, continuous positive airway pressure; CI, confidence interval; SO2, sulfur dioxide; NO2, nitrogen dioxide; O3, ozone.
Model calibration was evaluated using a calibration plot between observed (actual) risk and expected (predicted) risk which was shown in Figure 2.
Discussion
CPAP is a highly efficacious treatment of OSA which has been linked with a range of health conditions. The adherence of patients to this treatment is crucial for its overall effectiveness (2-4). Our study found no effect of an increase in PM10 and PM2.5 on low CPAP adherence in OSA patients. However, previous studies showed impaired sleep quality caused by air pollution (15-20) and the association of PM and the increasing of AHI both without and while using CPAP through the multiple hypotheses such as the upper airway irritation, the damage of airway epithelium and the changes in oxidative stress, the inflammation and autonomous nervous system control (15,16,19). From our explanatory research, we showed that the low CPAP adherence in subjects with OSA was not caused by the PM10 and PM2.5 but low adherence was associated with other factors including personal life issues and adverse attitudes towards CPAP treatment as well as health conditions which were supported by the previous study (8).
Our study is one of the discoveries in the pioneer era of air cleanness and OSA treatment using direct pollution levels to demonstrate the relationship and impact of air pollution especially PM10 and PM2.5 on CPAP adherence in subjects with OSA. However, we found no association between PM10 and PM2.5 on CPAP adherence. This could be explained that newer generation CPAP has more effective air filter system for inlet air purification, this factor might benefit the patient from the negative effects of the polluted air while using. However, further studies to explore the precise mechanism of the air quality and the CPAP tolerability in OSA patients are still required.
Our strength of this study is the first study on the effect of ambient air pollution on CPAP adherence in OSA patients. However, this study has some limitations. Firstly, the air pollution was measured at only one site that located in the central area of Chiang Mai, Thailand. Therefore, it may not be the same level across the entire area. However, all OSA subjects live in the same part of the country and all the pollution levels and exposure usually exceed the safety threshold defined by WHO during dry season (January–April) of the year. Secondly, monthly average of PM10 and PM2.5 and monthly average of CPAP adherence were used for analysis. This caused no association between PM10 and PM2.5 on CPAP adherence in our study. Therefore, the correlation between daily PM10 and PM2.5 and CPAP adherence should be focused in future studies.
Conclusions
Our study concluded that there was no an effect of PM10 and PM2.5 on low CPAP adherence in OSA patients. However, air purifiers should be still suggested for CPAP users during high air pollution periods for cardiorespiratory health benefits as demonstrated in previous studies.
Acknowledgments
The authors acknowledge the staff of the Sleep Disorders Center, Center for Medical Excellence, Faculty of Medicine, Chiang Mai University for their contribution to this trial. Finally, we acknowledge Ruth Leatherman, Research Administration Section, Faculty of Medicine, Chiang Mai University for native English proofreading.
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the series “Air Pollution” published in Journal of Thoracic Disease. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1507/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1507/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1507/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1507/coif). The series “Air Pollution” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University [Institutional Review Board (IRB) approval number: MED-2565-09282, date of approval 18 November 2022]. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- BaHammam AS. Comorbid depression in obstructive sleep apnea: an under-recognized association. Sleep Breath 2016;20:447-56. [Crossref] [PubMed]
- Cao MT, Sternbach JM, Guilleminault C. Continuous positive airway pressure therapy in obstuctive sleep apnea: benefits and alternatives. Expert Rev Respir Med 2017;11:259-72. [Crossref] [PubMed]
- Batool-Anwar S, Goodwin JL, Kushida CA, et al. Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA). J Sleep Res 2016;25:731-8. [Crossref] [PubMed]
- Theerakittikul T, Chaiard J, Deeluea J. Sleep quality, daytime sleepiness and daytime functioning among Thai obstructive sleep apnea patients receiving continuous positive airway pressure therapy. J Health Res 2021;36:972-82. [Crossref]
- Kohler M, Smith D, Tippett V, et al. Predictors of long-term compliance with continuous positive airway pressure. Thorax 2010;65:829-32. [Crossref] [PubMed]
- Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res 2010;131:245-58. [PubMed]
- Wells RD, Freedland KE, Carney RM, et al. Adherence, reports of benefits, and depression among patients treated with continuous positive airway pressure. Psychosom Med 2007;69:449-54. [Crossref] [PubMed]
- Tiyapun N, Sunkonkit K, Chaiwong W, et al. Factors influencing continuous positive airway pressure adherence in elderly with obstructive sleep apnea. J Thorac Dis 2023;15:3488-500. [Crossref] [PubMed]
- Bumroongkit C, Liwsrisakun C, Deesomchok A, et al. Correlation of Air Pollution and Prevalence of Acute Pulmonary Embolism in Northern Thailand. Int J Environ Res Public Health 2022;19:12808. [Crossref] [PubMed]
- Pothirat C, Chaiwong W, Liwsrisakun C, et al. The short-term associations of particular matters on non-accidental mortality and causes of death in Chiang Mai, Thailand: a time series analysis study between 2016-2018. Int J Environ Health Res 2021;31:538-47. [Crossref] [PubMed]
- Pothirat C, Chaiwong W, Liwsrisakun C, et al. Acute effects of air pollutants on daily mortality and hospitalizations due to cardiovascular and respiratory diseases. J Thorac Dis 2019;11:3070-83. [Crossref] [PubMed]
- Pothirat C, Chaiwong W, Liwsrisakun C, et al. Influence of Particulate Matter during Seasonal Smog on Quality of Life and Lung Function in Patients with Chronic Obstructive Pulmonary Disease. Int J Environ Res Public Health 2019;16:106. [Crossref] [PubMed]
- Pothirat C, Tosukhowong A, Chaiwong W, et al. Effects of seasonal smog on asthma and COPD exacerbations requiring emergency visits in Chiang Mai, Thailand. Asian Pac J Allergy Immunol 2016;34:284-9. [PubMed]
- Liwsrisakun C, Chaiwong W, Bumroongkit C, et al. Influence of Particulate Matter on Asthma Control in Adult Asthma. Atmosphere 2023;14:410. [Crossref]
- Kendzerska T, Szyszkowicz M, Alvarez JV, et al. Air Pollution and the Effectiveness of Positive Airway Pressure Therapy in Individuals With Sleep Apnea: A Retrospective Community-Based Repeated-Measures Longitudinal Study. Chest 2022;162:1176-87. [Crossref] [PubMed]
- Wang J, Wang W, Zhang W, et al. Co-exposure to multiple air pollutants and sleep disordered breathing in patients with or without obstructive sleep apnea: A cross-sectional study. Environ Res 2022;212:113155. [Crossref] [PubMed]
- Qiu H, Liu WT, Lin SY, et al. Association of air pollution exposure with low arousal threshold obstructive sleep apnea: A cross-sectional study in Taipei, Taiwan. Environ Pollut 2022;306:119393. [Crossref] [PubMed]
- Abou-Khadra MK. Association between PM10 exposure and sleep of Egyptian school children. Sleep Breath 2013;17:653-7. [Crossref] [PubMed]
- Cheng WJ, Liang SJ, Huang CS, et al. Air Pollutants Are Associated With Obstructive Sleep Apnea Severity in Non-Rapid Eye Movement Sleep. J Clin Sleep Med 2019;15:831-7. [Crossref] [PubMed]
- Wang J, Sun W, Wang W, et al. Association between exposure to air pollutants and sleep parameters in chronic obstructive pulmonary disease patients with or without obstructive sleep apnea. Chin Med J (Engl) 2022;135:2014-6. [Crossref] [PubMed]
- Shaukat R, Gamal Y, Ali A, et al. Adherence to Positive Airway Pressure Therapy in Patients With Obstructive Sleep Apnea. Cureus 2022;14:e25946. [Crossref] [PubMed]
- Pollution Control Department, Thailand. Reports on Smog Situation in the North Home page (in Thai). [Cited 2022 Dec 1]. Available online: http://www.pcd.go.th/
- Weather Information, Thai Meteorological Department. [Cited 2023 Dec 22]. Available online: https://www.tmd.go.th/en/


