High prevalence of gene abnormalities in young patients with lung cancer
Introduction
Many young patients with lung cancer at the time of diagnosis are already advanced stage and therefore result in a poor prognosis (1,2). For patients harboring the epidermal growth factor receptor (EGFR) gene mutation, EGFR tyrosine kinase inhibitors (EGFR-TKIs) have been used effectively to prolong progression-free survival and overall survival (3,4). Recently, the powerful driver oncogene, fusion gene of the anaplastic lymphoma kinase (ALK) with the echinoderm microtubule-associated protein-like 4 (EML4) was identified in non-small cell lung cancer (5). Prolongation of the survival period is expected with the use of the ALK-TKI. However, few studies have analyzed the frequency of driver oncogenes in young patients with non-small cell lung cancer aged 40 or younger. Therefore, we performed gene mutation analyses in young patients with lung cancer.
Methods and materials
We retrospectively reviewed medical records of all hospitalized patients with non-small cell lung cancer aged 40 or younger at Juntendo University Urayasu Hospital or Juntendo University Hospital from July 2004 to March 2010. We examined patient background, treatment modalities, and gene abnormalities. First, we examined EGFR mutation by performing direct sequencing for tumor biopsy specimens obtained by bronchoscope, resected tumor samples, or cell blocks of bronchoalveolar fluid or pleural effusion. When the EGFR mutation was negative, we next performed immunohistochemical analysis [using an intercalated antibody-enhanced polymer (iAEP)] and fluorescence in situ hybridization (FISH) for detection of the EML4-ALK fusion protein and gene (6), respectively. In negative cases for both EGFR mutation and EML4-ALK fusion gene, we analyzed the samples for presence of the K-ras mutation. We did not conduct re-evaluation for the EGFR gene mutation after recurrence. Survival analysis was conducted using the Kaplan-Meier method.
Results
Case profile
We retrospectively studied 12 young patients with non-small cell lung cancer (men, 7; women, 5). The mean age of the patients was 35.3 years (Table 1).
Table 1
| No | Age | Sex | BI | Histology | T | N | M | Stage | PS | EGFR | EML4-ALK | 1st line | 2nd line | Outcome | Survival time |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 33 | m | 10 | adeno | 4 | 0 | 1 | IV | 1 | + | n.d. | CBDCA+TXL | Gefitinib | death | 1,208 days |
| 2 | 37 | m | 800 | adeno | 4 | 2 | 1 | IV | 1 | + | n.d. | Gefitinib | CBDCA+TXL | death | 461 days |
| 3 | 37 | m | 450 | adeno | 4 | 3 | 1 | IV | 3 | + | n.d. | CBDCA+TXL | Gefitinib | death | 379 days |
| 4 | 39 | m | 400 | adeno | 3 | 3 | 1 | IV | 0 | + | n.d. | CDDP+PEM | Gefitinib | death | 364 days |
| 5 | 31 | f | 100 | adeno | 1 | 3 | 0 | IIIB | 0 | ± | n.d. | CBDCA+TXL | Gefitinib | alive | 2,688+α |
| 6 | 35 | f | 0 | adeno | 4 | 0 | 0 | IIIB | 0 | - | + | CBDCA+GEM | PEM | alive | 1,456+α |
| 7 | 37 | f | 0 | adeno | 2 | 1 | 1 | IV | 0 | - | + | CBDCA+PEM | alive | 757+α | |
| 8 | 34 | f | 0 | adeno | 4 | 3 | 1 | IV | 2 | - | + | CBDCA+TXL | GEM | death | 568 days |
| 9 | 33 | m | 300 | adeno | 4 | 3 | 1 | IV | 1 | - | + | CBDCA+TXL | CBDCA+PEM | death | 175 days |
| 10 | 35 | m | 0 | adeno | 4 | 3 | 1 | IV | 1 | - | + | CBDCA+TXL | CBDCA+PEM | death | 99 days |
| 11 | 37 | f | 0 | adeno | 2 | 2 | 0 | IIIA | 0 | - | - | CBDCA+TXL | alive | 365+α | |
| 12 | 36 | m | 340 | non-small | 2b | 3 | 1b | IV | 1 | - | - | CBDCA+TXL | alive | 280+α |
Abbreviations: BI, brinkman index; PS, performance status; ±, EGFR mutaion indeterminate, but responded to gefitinib; n.d., not done; CBDCA, carboplatin; TXL, pacritaxicel; PEM, pemetrexed; GEM, gemcitabine.
Smoking history
Six patients were smokers. Three out of these patients were heavy smokers over 20 pack pear, and had a long history of smoking. One man and 4 women were non-smokers.
Histology and stage of the disease
All of the patients had non-small cell lung cancer. Eleven patients (91.6%) were diagnosed with adenocarcinoma, while one was with histology not otherwise specified. According to the clinical TMN classification, there were 1 patient with stage IIIA, 2 with stage IIIB cancer; and 9 with stage IV.
Examination of the gene abnormalities
Activating EGFR gene mutations, exon 19 deletion, were detected in 4 cases.
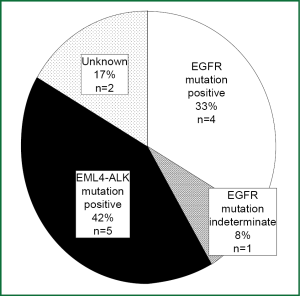
One case whose EGFR gene mutations were indeterminate because sample size was not enough for direct sequencing. But she seems to harbor EGFR activation mutation because she responded to gefitinib remarkably. Therefore, we considered that she harbored an EGFR mutation. Subsequently, we conducted iAEP followed by FISH analyses for 7 patients without EGFR mutation to determine EML4-ALK fusion protein and gene. Among 7 patients, 5 patients showed positive for EML4-ALK protein or gene. Analysis for the presence of K-ras mutation was performed in 2 cases that were negative for both the EGFR mutation and the EML4-ALK fusion gene. One of the cases was K-ras mutation-negative, while the other case was not clear for K-ras mutation because of inadequate sample (Figure 1).
Median survival time and survival curve
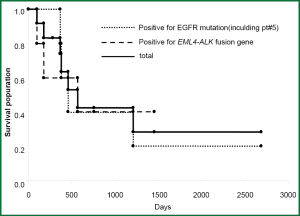
The patients harboring EGFR mutation were treated with gefitinib. The median survival time (MST) was 461 days. The MST for the patients harboring EML4-ALK fusion gene was 568 days (Figure 2), because these patients could not be treated ALK inhibitors.
Discussion
In this study, all patients were diagnosed as non-small cell lung cancer with advanced stage. Development of metastases without symptoms or prolonged neglect of symptoms could be the reasons for this finding. Gene analysis showed that EGFR mutation was clearly identified in 4 of our 12 cases.
The frequency of the EGFR mutation in cases of lung adenocarcinoma has been reported by a previous study (7). There were no significant differences in the frequency for EGFR mutation depending on the patient age (8). Five of the 7 EGFR-negative cases in our study were detected to have the EML4-ALK fusion gene. According to a previous study, the frequency of the EML4-ALK fusion gene is in the range of 1.6% to 8.6% (9-12). The EML4-ALK fusion gene is recognized to be associated with the onset of lung cancer in young patients. EML4-ALK fusion gene has an exclusive relation with EGFR mutation and K-ras mutation (13). The frequency for the EML4-ALK fusion gene in this study was markedly higher than previous studies. Our sample-size was small, but gene abnormalities were identified in 75% in patients aged 40 and younger with lung cancer. Although all patients with EGFR activating mutation were treated with an EGFR-TKI, the overall survival was unsatisfactory. Unfortunately, we did not perform a re-examination for the gene abnormalities in the recurrent tumors. One of the potential mechanisms for short survival for these patients could be explained by the fact that 3 patients were heavy smokers, whose k-ras could be mutated. Moreover, we could evaluate only one case the k-ras status. Furthermore, the overall survival of the patients harboring the EML4-ALK fusion gene was also unsatisfactory, probably because ALK-TKI was not available at that time for these patients.
The results indicated that driver oncogenes were detected in 75% of our cases and that the frequency of EML4-ALK fusion gene was high in the young patients with non-small cell lung cancer. Our finding also suggests that the onset of non-small cell lung cancer in patients aged 40 or younger is more significantly related to gene abnormalities including driver oncogene mutation than to environmental factors.
Conclusions
In this study, we clarified that all 12 patients aged 40 and younger were non-small cell lung cancer and 9 in 12 patients were positive for the EGFR gene mutation or the EML4-ALK fusion gene. Our study revealed that ALK fusion gene affected carcinogenesis by the young patients in efficiency more than previous reports. Therefore, examination of gene abnormalities is especially important in young patients with lung cancer to provide an appropriate treatment modality.
Acknowledgements
We would like to thank Dr. Takeuchi, PhD, Pathology Project for Molecular Targets, the Cancer Institute, Japanese Foundation for Cancer Research, for detecting the EML4-ALK fusion gene by using the iAEP and FISH methods.
Disclosure: The authors declare no conflict of interest.
References
- Jubelirer SJ, Wilson RA. Lung cancer in patients younger than 40 years of age. Cancer 1991;67:1436-8. [PubMed]
- Larrieu AJ, Jamieson WR, Nelems JM, et al. Carcinoma of the lung in patients under 40 years of age. Am J Surg 1985;149:602-5. [PubMed]
- Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 2005;353:123-32. [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [PubMed]
- Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561-6. [PubMed]
- Takeuchi K, Choi YL, Togashi Y, et al. KIF5B-ALK, a novel fusion oncokinase identified by an immunohistochemistry-based diagnostic system for ALK-positive lung cancer. Clin Cancer Res 2009;15:3143-9. [PubMed]
- Mitsudomi T, Yatabe Y. Mutations of the epidermal growth factor receptor gene and related genes as determinants of epidermal growth factor receptor tyrosine kinase inhibitors sensitivity in lung cancer. Cancer Sci 2007;98:1817-24. [PubMed]
- Toyooka S, Takano T, Kosaka T, et al. Epidermal growth factor receptor mutation, but not sex and smoking, is independently associated with favorable prognosis of gefitinib-treated patients with lung adenocarcinoma. Cancer Sci 2008;99:303-8. [PubMed]
- Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J Thorac Oncol 2008;3:13-7. [PubMed]
- Takahashi T, Sonobe M, Kobayashi M, et al. Clinicopathologic features of non-small-cell lung cancer with EML4-ALK fusion gene. Ann Surg Oncol 2010;17:889-97. [PubMed]
- Martelli MP, Sozzi G, Hernandez L, et al. EML4-ALK rearrangement in non-small cell lung cancer and non-tumor lung tissues. Am J Pathol 2009;174:661-70. [PubMed]
- Paik JH, Choe G, Kim H, et al. Screening of anaplastic lymphoma kinase rearrangement by immunohistochemistry in non-small cell lung cancer: correlation with fluorescence in situ hybridization. J Thorac Oncol 2011;6:466-72. [PubMed]
- Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK lung cancers are characterized by rare other mutations, a TTF-1 cell lineage, an acinar histology, and young onset. Mod Pathol 2009;22:508-15. [PubMed]