Prolonged postoperative length of stay is associated with poor overall survival after an esophagectomy for esophageal cancer
Introduction
Surgery remains the mainstay of treatment for patients with early or locally advanced esophageal cancer (EC). The operative approach of extended esophagectomy with 3-field lymph node dissection (3FLND) provides the highest potential for a cure (1,2). However, an esophagectomy as a treatment for cancer is a major surgical procedure that is associated with high morbidity and mortality rates (3,4). Several studies have suggested that postoperative complications might exert a negative influence on the long-term survival of patients. It is imperative to explore the exact reasons for these adverse effects.
Previous studies mainly focused on detailed postoperative complications, such as respiratory complications (5,6) or anastomotic leak (7,8). However, while these studies described the relationship between a certain complication and long-term survival, they failed to explain the underlying causes or to delineate the magnitude of risk for the particular adverse effect studied. In comparison, postoperative length of hospital stay is a relatively objective index that directly impacts the postoperative rehabilitation of patients. The aim of the current study was to contribute to the discussion regarding the impact of postoperative length of stay (LoS) on long-term outcomes in patients who underwent an esophagectomy with 3FLND at a single, experienced, high-volume center.
Patients and methods
Patients
A total of 364 EC patients who underwent an esophagectomy at Fudan University Shanghai Cancer Center from January 2001 to December 2009 were enrolled in this study. The inclusion criteria for this study were as follows: pathologically confirmed thoracic esophageal squamous carcinoma; only one primary tumor; no neoadjuvant chemotherapy and/or radiotherapy; and tumor-free resection margins as determined by microscopic examination of the surgical specimen. All of the enrolled patients were diagnosed with EC by endoscopic biopsy. Preoperative staging was determined mainly by enhanced chest computerized tomography and ultrasonography/computed tomography of the neck and abdomen. Stage T1-T3 EC patients were selected as candidates for operation. A physical examination, standard laboratory tests, electrocardiograms, and lung function tests were performed on all of the enrolled patients.
All of the enrolled patients received a combination of epidural and general anesthesia before the operation. The operative technique used for an esophagectomy with 3FLND has been previously described (9,10). The operation consisted of a right thoracotomy, laparotomy, and a collar neck incision. A thoracotomy is usually performed at the right fourth or fifth intercostal space through either a posterolateral or small incision. The patients stayed overnight in the surgical intensive care unit (ICU) on continuous telemetry before returning to the dedicated thoracic surgical ward on the first postoperative day. This study was approved by the Institutional Review Board.
Statistical analysis
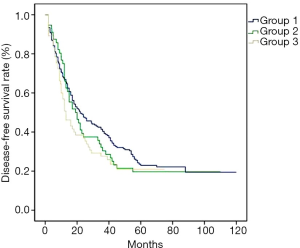
Overall survival (OS) was computed from the date of surgery using Kaplan-Meier estimates. A log-rank test was used to assess the equality of survival functions. To determine the effect of postoperative LoS on long-term survival, we separated the patients into three groups based on the length of postoperative LoS: LoS of less than 2 weeks (Group 1, ≤2 W), LoS of between 2 and 3 weeks (Group 2, ≤3 W) and LoS of more than 3 weeks (Group 3, >3 W). Differences were assessed using a Wilcoxon rank sum test for continuous variables, chi-square or Fisher exact tests for categorical variables, Kaplan-Meier method for survival time, and multivariate Cox regression analyses to adjust for age, sex, tumor location, pathological TNM stage, and adjuvant therapy. Variables with P values less than 0.10 by univariate analyses were included in the multivariate analyses. For all calculations, a P value of <0.05 was considered significant. Statistical computations and plotting were performed using SPSS software, version 19.0 (SPSS, Chicago, IL).
Results
Patient demographics
A total of 364 patients met the criteria for inclusion in this study. Of these patients, 16 were excluded from the analysis because of perioperative death (3 cases) or because they were lost to follow-up after surgery (13 cases). The characteristics of the remaining 348 patients are summarized in Table 1. The cohort was predominately male, with 281 men and 67 women. The mean age at time of surgery was 57.8±7.7 years. There were no significant differences in age (P=0.107), sex (P=0.399), body mass index (BMI) (P=0.970), smoking history (P=0.278), alcohol history (P=0.104), or comorbidity (P=0.174) among three groups. According to the Union for International Cancer Control (UICC) EC TNM staging system (7th Edition, 2010), there were 61 cases of postoperative TNM stage 1 (17.5%), 113 cases of postoperative TNM stage 2 (32.5%), and 174 cases of postoperative TNM stage 3 (50.0%) in our study. There were no significant differences in tumor location (P=0.053) or postoperative TNM stage (P=0.900) among the three groups.
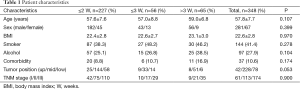
Full table
Operative features and morbidity
All of the enrolled patients underwent an esophagectomy with 3FLND. The mean operative time was 4.4±1.0 hours, the mean volume of blood lost was 243±141 mL, and the median postoperative hospital stay was 14 days (range: 8-153 days). Complications were observed in 123 patients (15.9% in Group 1 vs. 73.2% in Group 2 vs. 96.6% in Group 3, P<0.001). The detailed operative features and morbidity are listed in Table 2.
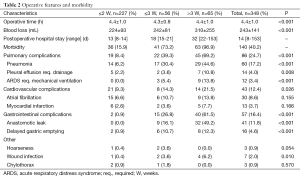
Full table
Survival
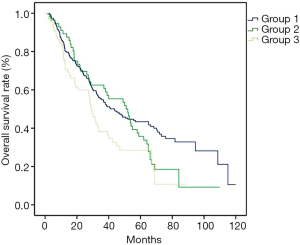
The median duration of follow-up was 39 months (range: 3-120 months). Tumor details, relevant postoperative adjuvant therapy and survival rates are shown in Table 3. No significant differences were found in T stage, vessel invasion or nerve invasion of the tumor, lymph node status, nodal yield, postoperative chemotherapy, radiotherapy or chemoradiotherapy among the three groups. Significant reductions in preventive adjuvant therapy (P=0.003) and postoperative salvage therapy (P<0.001) were observed among the three groups. The 5-year survival rate was significantly different among the groups (43% vs. 36% vs. 29%, P=0.006) (Figure 1). There were no significant differences in the 5-year disease-free survival rate among the three groups (23% vs. 21% vs. 19%, P=0.238) (Figure 2).
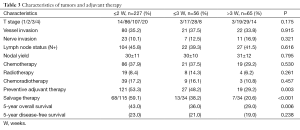
Full table
Discussion
The present study demonstrated a lower OS rate of patients who experienced a prolonged postoperative LoS. The patients in the prolonged HS group were more likely to receive less preventive adjuvant therapy and salvage therapy after a recurrence of their tumor, which could contribute to our results.
Because it involves the reconstruction of the digestive tract, surgery for EC is associated with multiple types of postoperative complications, and the overall incidence of complications is relatively high (11). Over the past decade, researchers in Western countries have become increasingly concerned about the impact of post-surgery related complications on long-term survival (12-15). Because of the various definitions of complications after EC surgery used in different studies, complications are categorized as medical complications and surgical/technical complications (2,5,12,14,15), as minor and major complications (16), or as complications according to the organ systems involved, referring to the Society of Thoracic Surgeons (STS) database (7). Accordingly, previous studies focused on the relation between complications and long-term survival as well as the relation between readmissions and long-term survival (17). The conclusions of these studies were therefore not always consistent (5,7,13,16). Even a single complication, such as common pneumonia or anastomotic leakage, could occur at various magnitudes ranging from mild to critical and have various impacts on the immune system and quality of life (14,15). Thus, a universal index is necessary to assess the relation between surgical trauma and long-term survival. The postoperative length of hospital stay is an objective parameter that can accurately reflect the postoperative recovery of a patient. The aim of the current study was to contribute to the discussion on the impact of postoperative LoS on the long-term outcomes of patients who underwent an esophagectomy with 3FLND at a single, experienced, high-volume center.
Because squamous cell carcinoma (SCC) presents with early lymphatic spread, a high location in the esophagus, and a poor prognosis (18), a radical resection is complicated in cases of SCC. Compared with its history in Western countries (16,19), the histology of EC in Asian populations is predominantly SCC rather than adenocarcinoma. Obviously, most studies in the Western world cannot match the characteristics of etiology and metastasis observed in Asian patients with EC. Therefore, it is necessary to further stratify the characteristics of patients with SCC.
The reason that prolonged LoS poses such a negative effect on long-term outcomes might be insufficient postoperative oncologic therapy. The general level of physical performance after a prolonged LoS may be so poor that postoperative oncologic therapy would be delayed, or even canceled, by doctors or patients. Thus, patients with a long LoS are at a survival disadvantage. Krarup and colleagues (20) have suggested that the cancelled or delayed administration of adjuvant chemotherapy might partly account for the increased rates of distant recurrence seen in patients with anastomotic leakage after colonic cancer resection. Patients who experience a prolonged LoS, especially those with an LoS longer than 3 weeks, would also find that the long LoS negatively affects their self-confidence and confidence in their ability to fight a tumor. A prolonged LoS may also undermine the trust relationship between physician and patient. Therefore, upon relapse of their disease, a patient’s desire to receive salvage therapy could be compromised. The present study also found significant reductions in the rates of administration of preventive adjuvant therapy and salvage therapy in patients with a long LoS.
A major limitation of this retrospective study is the lack of follow-up for immunologic markers. Studies have demonstrated that perioperative complications can suppress immune function in patients with EC after surgery and thus negatively affect rates of tumor relapse rather than OS (15). However, those studies’ results are not consistent with our findings. Further research on this topic is necessary to clarify these differences. Another limitation of this study is the exclusion of patients who died during their early postoperative courses. Early postoperative mortality affects general outcomes. However, we aimed to assess the impact of prolonged LoS on long-term outcomes. Therefore, we excluded in-hospital deaths from our analysis, as described in the literature (7,15,16).
In conclusion, the present study demonstrates increased mortality rates in patients who underwent an intended curative EC resection and survived a prolonged LoS. The excess long-term mortality observed in the present study requires further investigation. A prolonged LoS may indicate a long recovery time, and the window of opportunity in which to receive effective adjuvant therapy may be missed in these cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Berry MF. Esophageal cancer: staging system and guidelines for staging and treatment. J Thorac Dis 2014;6 Suppl 3:S289-97. [PubMed]
- Krengli M, Sedlmayer F, Calvo FA, et al. ISIORT pooled analysis 2013 update: clinical and technical characteristics of intraoperative radiotherapy. Transl Cancer Res 2014;3:48-58.
- Ye T, Sun Y, Zhang Y, et al. Three-field or two-field resection for thoracic esophageal cancer: a meta-analysis. Ann Thorac Surg 2013;96:1933-41. [PubMed]
- Ashtari S, Vahedi M. Economic burden of gastrointestinal cancer: estimation and importance. Transl Gastrointest Cancer 2014;3:178-81.
- D’Annoville T, D’Journo XB, Trousse D, et al. Respiratory complications after oesophagectomy for cancer do not affect disease-free survival. Eur J Cardiothorac Surg 2012;41:e66-73; discussion e73.
- Yano T, Hatogai K, Morimoto H, et al. Photodynamic therapy for esophageal cancer. Ann Transl Med 2014;2:29. [PubMed]
- Kofoed SC, Calatayud D, Jensen LS, et al. Intrathoracic anastomotic leakage after gastroesophageal cancer resection is associated with increased risk of recurrence. J Thorac Cardiovasc Surg 2015;150:42-8. [PubMed]
- Akl FM, Elsayed-Abd-Alkhalek S, Salah T. Palliative concurrent chemoradiotherapy in locally advanced and metastatic esophageal cancer patients with dysphagia. Ann Palliat Med 2013;2:118-23. [PubMed]
- Li H, Zhang Y, Cai H, et al. Pattern of lymph node metastases in patients with squamous cell carcinoma of the thoracic esophagus who underwent three-field lymphadenectomy. Eur Surg Res 2007;39:1-6. [PubMed]
- Fujita H, Sueyoshi S, Tanaka T, et al. Three-field dissection for squamous cell carcinoma in the thoracic esophagus. Ann Thorac Cardiovasc Surg 2002;8:328-35. [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [PubMed]
- Rizk NP, Bach PB, Schrag D, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 2004;198:42-50. [PubMed]
- Abou-Jawde RM, Mekhail T, Adelstein DJ, et al. Impact of induction concurrent chemoradiotherapy on pulmonary function and postoperative acute respiratory complications in esophageal cancer. Chest 2005;128:250-5. [PubMed]
- Lagarde SM, de Boer JD, ten Kate FJ, et al. Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg 2008;247:71-6. [PubMed]
- Lerut T, Moons J, Coosemans W, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg 2009;250:798-807. [PubMed]
- Lindner K, Fritz M, Haane C, et al. Postoperative complications do not affect long-term outcome in esophageal cancer patients. World J Surg 2014;38:2652-61. [PubMed]
- Fernandez FG, Khullar O, Force SD, et al. Hospital readmission is associated with poor survival after esophagectomy for esophageal cancer. Ann Thorac Surg 2015;99:292-7. [PubMed]
- Siewert JR, Ott K. Are squamous and adenocarcinomas of the esophagus the same disease? Semin Radiat Oncol 2007;17:38-44. [PubMed]
- Carrott PW, Markar SR, Kuppusamy MK, et al. Accordion severity grading system: assessment of relationship between costs, length of hospital stay, and survival in patients with complications after esophagectomy for cancer. J Am Coll Surg 2012;215:331-6. [PubMed]
- Krarup PM, Nordholm-Carstensen A, Jorgensen LN, et al. Anastomotic leak increases distant recurrence and long-term mortality after curative resection for colonic cancer: a nationwide cohort study. Ann Surg 2014;259:930-8. [PubMed]


