Covering the staple line with a polyglycolic acid sheet after bullectomy for primary spontaneous pneumothorax prevents postoperative recurrent pneumothorax
Introduction
Bullectomy is often performed as a video-assisted thoracic surgery (VATS)-based treatment for recurrent pneumothorax and pneumothorax involving prolonged air leakage (1-8), but it seems to result in a higher frequency of postoperative recurrent pneumothorax (PORP) than conventional thoracotomy methods (lateral thoracotomy or axillary thoracotomy) (9-12). To prevent PORP, additional therapies aimed at achieving pleural adhesion, such as performing pleurectomy after bullectomy, spraying talc within the chest cavity, or administering certain antibiotics into the chest cavity, have been examined and shown to be effective (13-22). In recent years, evidence has accumulated that the application of a covering material along the resection line after bullectomy is effective at preventing PORP (23-27). In this study, the factors associated with PORP are studied as well as the efficacy of covering the visceral pleura with a PGA sheet as a treatment for preventing PORP.
Materials and methods
Patients
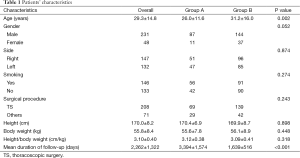
Among the 265 patients (279 cases) with primary spontaneous pneumothorax (PSP) who underwent surgery at Nippon Medical School Chiba Hokusoh Hospital between April 1994 and December 2007, the cases of 92 patients (98 cases) that underwent bullectomy alone before September 2002 (group A) and 173 patients (181 cases) who underwent bullectomy followed by covering of the visceral pleura with a PGA sheet in October 2002 or later (group B) were reviewed retrospectively. The patients’ characteristics are shown in Table 1. The patients included 231 males and 48 females, and their mean age was 29.3±14.8 years old. There were 87 males and 11 females in group A, and their mean age was 26.0±11.6 years old. The patients in group A underwent bullectomy alone. In addition, there were 144 males and 37 females in group B, and their mean age was 31.2±16.0 years old. In group B, bullectomy was performed, and then the staple line and the surrounding visceral pleura were covered with a PGA sheet. Surgery was performed simultaneously on both sides in 14 cases. When the same patient underwent surgery on both sides, each side was treated as a separate case. Similarly, when postoperative recurrence was observed twice on the same side in the same patient each recurrent episode was treated as a separate case.
Full table
Operative procedure
At our institution, surgery is mainly performed for the following types of pneumothorax: cases of recurrent pneumothorax in which bullae are observed in the lungs on CT or cases of primary pneumothorax involving prolonged air leakage (for ≥5 days) after the start of chest cavity drainage. In all cases, a double lumen endotracheal tube was inserted into the airway under general anesthesia, and surgery was performed during selective ventilation of the contralateral lung. In all cases, surgery was carried out whilst the patient was in the lateral position. As for the thoracotomy method, thoracoscopic surgery (TS) was performed in 208 cases, axillary thoracotomy was carried out in 49 cases, lateral thoracotomy (>10 cm) was employed in 14 cases, and TS + minithoracotomy (<10 cm) was performed in 8 cases. TS was performed using the three-port method. In this method, the first 2 cm port is created along the anterior axillary line of the fifth or sixth intercostal space, and then two 0.5 or 1.5 cm ports are created in the chest wall according to the degree of adhesion and the locations of any bullae. A careful search for bullae was performed by examining the surface of the visceral pleura, and a leak test was simultaneously conducted at a pressure of 20 cmH2O in order to check for air leakage. After bullectomy of any bullae observed on the lung surface using an endoscopic stapling device [either an Autosuture GIA Universal, Tyco Healthcare (Convidien), Norwalk, CT, USA, or an Endopath ETS45, Ethicon Endo-Surgery, Cincinnati, OH, USA, depending on the surgeon’s preference], another leak test was conducted at an airway pressure of 20 cmH2O in order to confirm that there was no air leakage from the resection line, etc. In Group B, a PGA sheet (either an DexonTM Mesh, Syneture, USA, or Neoveil, Gunze, Kyoto, Japan, depending on the surgeon’s preference) that had been cut to an appropriate size (approximately 5 cm × 5 cm) was inserted through the relevant port and was used to cover the surface of the visceral pleura around the staple line. Fibrin glue was used to fix the sheet in place. A 20 Fr chest tube was inserted through one of the ports and connected to a continuous suction system, and continuous suction was performed at a negative pressure of 10 cmH2O. After it was confirmed that there was no air leakage and good re-expansion of the lungs had been confirmed on a chest X-ray, the chest tube was generally removed on postoperative day 1.
Statistical analysis
All data in the text and tables are expressed as mean ± SD values. All statistical analyses were performed using the software SPSS (SPSS for Windows v. 15, SPSS, Inc. Chicago, IL, USA). Comparisons of the patients’ characteristics were made using the two-tailed Student’s t-test or chi-square test.
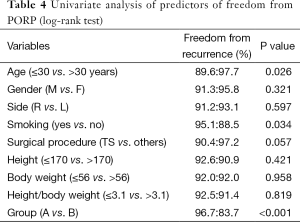
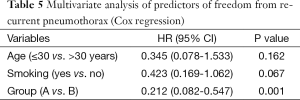
Univariate analyses (log-rank test) were performed to examine the associations between PORP and age, gender, the affected side, smoking habits, surgical procedure, height, body weight, height/weight ratio, or the application of a PGA sheet, and multivariate analysis (using the Cox proportional hazards method) was performed to extract independent prognostic factors from among the parameters that demonstrated significant associations in the univariate analysis.
P values of <0.05 were considered to indicate statistical significance for all parameters.
Results
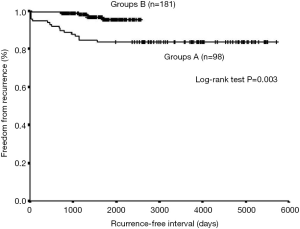
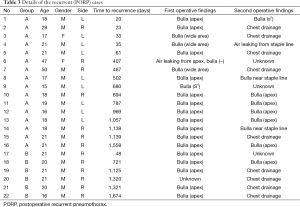
After October 2002, when the covering procedure was introduced, the mean age of the patients who underwent surgery for PSP increased significantly (P=0.002). No significant differences were observed between the groups in terms of gender, the affected side, height, body weight, height/weight ratio, smoking habits, or surgical procedure (Table 1). The mean duration of the follow-up period was 3,394±1,574 days in group A and 1,639±516 days in group B. No surgery-related deaths occurred after the first or second surgical procedures in either group. The patients who developed PORP underwent a consultation after the first surgical procedure, during which they presented with chest pain and respiratory discomfort as major complaints, and recurrent pneumothorax was confirmed on a chest X-ray. PORP occurred in a total of 22 cases (7.9%), including 16 (16.3%) and 6 (3.3%) cases in groups A and B, respectively. The time until the development of PORP was less than 2 months in 6 cases, 3 to 12 months in 0 cases, 13 to 24 months in 5 cases, and ≥25 months in 11 cases (Figure 1). The characteristics of the recurrent and non-recurrent cases are shown in Table 2, and further details about the recurrent cases are shown in Table 3. A second surgical procedure was performed in 13 patients in whom bullae were observed on CT and air leakage occurred for ≥5 days after chest drainage. Eleven of these patients belonged to group A, and the other 2 were in group B. The remaining 9 patients who suffered PORP exhibited improvements in their conditions after chest cavity drainage, and therefore, did not undergo further surgery. Bullae were observed during the second surgical procedure in a total of 9 cases, including 8 of the 11 cases (73%) in group A and 1 of the 2 cases (50%) in group B. Of these, it is considered that the bullae found in patient 1, who suffered recurrence on postoperative day 20, had been overlooked during the original procedure, but in the other 8 cases the bullae were detected at ≥13 postoperative months, and therefore, it was difficult to determine with any degree of certainty whether they had been overlooked during the original operation or had developed during the postoperative period. Regarding other types of recurrence, air leakage from the area near to the staple line was observed in 1 case, air leakage from a pinhole in the visceral pleura was observed in 1 case, and PORP of unknown cause was seen in 3 cases (Table 3). Age, gender, the affected side, height, body weight, height/weight ratio, smoking habits, surgical procedure (TS vs. others), and the application of a PGA sheet were considered as factors that might affect the risk of recurrence. According to univariate analysis, the cumulative recurrence-free rate was highest among the patients that were ≥30 years old, smokers, and those in which the visceral pleura was covered with a PGA sheet (group B) (Table 4). A multivariate analysis involving these three items was performed, and only the covering of the visceral pleura with a PGA sheet was found to be an independent prognostic factor (Table 5). Kaplan-Meier curves for group A and group B are presented in Figure 2.


Full table
Full table
Full table
Full table
Discussion
Surgical treatment used to be selected for prolonged air leakage or recurrent pneumothorax (28), but in recent years bullectomy using an endoscopic stapling device has been widely performed as a VATS-based procedure for such conditions due to its low degree of invasiveness (1-8). However, PORP, which frequently occurs after open thoracotomy, has become a problem (9-12). In the present study, the mean age of the patients who underwent surgery for PSP was 29.3 years old (Table 4), and that of the patients who developed PORP was 22.3 years old (Table 2), which indicates that both of these conditions predominantly affect young subjects. PSP and PORP are not life-threatening disorders, but as they occur at an age when many individuals are experiencing important life events such as entrance examinations for university, they can cause patients serious social disadvantages. Therefore, it is necessary to continuously make an effort to decrease the incidence of PORP.
In our study, when the time at which PORP occurred and the number of cases of PORP were plotted on a graph focusing on the presence of bullae during the second surgery, 2 peaks were observed (Figure 1). In other words, PORP mainly developed within 2 months after surgery (early) or >1 year after surgery (late), and no cases of PORP occurred between 3 and 12 postoperative months. A bulla was observed during the second surgical procedure in 1 of the 3 cases (33%) in which PORP occurred early in the postoperative period, and it was considered that it had been overlooked during the initial procedure. On the other hand, bullae were observed during the second surgical procedure in 8 of the 10 cases (80%) in which PORP occurred after >1 year after surgery (Table 3). Based on the timing and pattern (the presence/absence of bullae during the second surgery) of these PORP cases, it is possible that cases of PORP that occur early and late after surgery for PSP are caused by different mechanisms.
Intraoperative damage to the visceral pleura and the overlooking of bullae are considered to be potential causes of early PORP (17). Bullae can be overlooked due to endoscopic blind spots or intraoperative pulmonary collapse caused by separate ventilation (13). In order to prevent early PORP, it is important to prevent air leakage from areas of damaged visceral pleura and to avoid overlooking bullae during the initial procedure. In our series, the visceral pleura were not covered with a PGA sheet in 5 of the 6 cases (83%) in which PORP occurred early after surgery.
Previous studies have also reported the detection of bullae during surgery for PORP (14,22-25,27), and bullae were observed in 9 of the 13 cases (69%) in which second surgical procedures were performed for PORP in our study (Table 3). Among these 9 cases, with the exception of 1 case in which it was considered that the bulla had been overlooked during the first procedure, all 8 cases involved late PORP. In the latter 8 cases, it was difficult to determine whether the bullae observed during the second surgical procedures had been overlooked during the initial procedure or had subsequently developed. However, during the first procedure at least two people, including the operator and the supervisor, carefully observed the surface of the visceral pleura, and it is difficult to believe that all of these cases of PORP were due to the overlooking of bullae. In particular, we consider that the cases of PORP in which bullectomy were performed during the first procedure and bullae developed close to the staple line were caused by the rupturing of regenerated bullae. It is considered that bullae regeneration requires a certain amount of time, but no bullae were observed in any of the cases of early PORP other than the case in which it was considered that a bulla had been overlooked during the initial procedure. On the other hand, bullae were observed in 80% of the cases of late PORP, and therefore, it can be speculated that bullae regeneration contributes to PORP. It is suggested that weakening of the pleura due to the tensional force applied to the visceral pleura and/or the deformation of fine bronchial tubes due to the tensional force applied to the lung by staples, etc., are responsible for bullae regeneration (7,26,27). It is considered that it is necessary to prevent the regeneration and rupturing of bullae in order to avoid the late occurrence of PORP. In our series, the visceral pleura were not covered with a PGA sheet in 11 of the 16 cases (69%) in which late PORP developed.
The covering of the staple line with an absorbefacient sheet has been reported to be effective against PORP. In the present study, the covering of the visceral pleura with an absorbefacient sheet was found to be an independent prognostic factor (Table 5), indicating that this method helps to prevent PORP early and late after surgery. Similarly, methods in which absorbefacient sheets were held in place with fibrin glue (23-26) or in which the staple line was reinforced with fleece-coated fibrin glue (TachoComb) (27) have also been reported to be effective against PORP. The application of fleece-coated fibrin glue close to the resection line has been reported to reduce the frequency of PORP to a similar level to that achieved by the use of absorbefacient sheets (27). Fleece-coated fibrin glue requires a few minutes of compression when it is used to bind the visceral pleura, and it is considered that it is difficult to redo such procedures if they fail. On the other hand, PGA sheets are easy to use in operations both in terms of their insertion through ports and their application, and it is considered that procedures involving PGA sheets can be redone if they fail. Although methods involving fibrin glue or fleece-coated fibrin glue have been demonstrated to inhibit PORP, both of these adhesives are derived from blood and so carry a risk of viral infection (29). In recent years, in order to eliminate the possibility of viral infection, different methods such as the application of PGA sheets using autologous blood (30,31) and other materials (32) and the fixation of PGA sheets to the visceral pleura using absorbefacient thread (33) have been reported. When these methods are employed, it takes a while to determine the strength of the fixation between the sheet and the target tissue and whether the sheet remains fixed to the intended site while it is being stretched. As it is impossible to confirm whether a sheet covers the intended area while it is being stretched during lung re-expansion using postoperative X-rays or CT scans, the long-term prognoses of such procedures need to be compared and investigated in the future in order to compare their relative merits. If the use of alternative adhesives such as autologous blood results in similar long-term prognostic outcomes to those seen after the use of fibrin glue, then PGA sheets should be fixed in place with these alternatives. Until then, our policy is to continue using fibrin glue. Sakamoto et al. (23) reported that in cases of PSP in which artificial absorbefacient sheets, such as PGA sheets, were used, thickening associated with fibrosis of the visceral pleura was observed in the resected lung specimens obtained during the second surgical procedure. In our study, no pathological analysis was conducted as no resected specimens of the covered regions of the pleura were obtained during the second surgical procedures in Group B. On the other hand, Nakanishi et al. (24) recently reported that no thickening of the pleura or associated reinforcement occurred when absorbefacient sheets were fixed to the visceral pleura with fibrin glue, and it is speculated that the inflammatory reaction induced in the pleura by the absorbefacient sheets promoted their adhesion to the visceral pleura and the parietal pleura, and thereby, reduced the risk of PORP. Furthermore, it was pathologically confirmed that bullae regeneration occurs in the layer underneath the area covered by the absorbefacient sheet. Therefore, it is speculated that PGA sheets prevent PORP by stopping recurrent bullae from rupturing, rather than by inhibiting bullae generation.
In conclusion, according to the findings of both previous reports and this study, it is considered that covering large portions of the staple line and the surrounding region with a PGA sheet after bullectomy prevents both early PORP, which is associated with damage to the visceral pleura in the regions close to the resection line; air leakage from the staple line; and late PORP, which is related to the recurrence of bullae >1 year after surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [PubMed]
- Naunheim KS, Mack MJ, Hazelrigg SR, et al. Safety and efficacy of video-assisted thoracic surgical techniques for the treatment of spontaneous pneumothorax. J Thorac Cardiovasc Surg 1995;109:1198-203; discussion 1203-4.. [PubMed]
- Mouroux J, Elkaïm D, Padovani B, et al. Video-assisted thoracoscopic treatment of spontaneous pneumothorax: technique and results of one hundred cases. J Thorac Cardiovasc Surg 1996;112:385-91. [PubMed]
- Hazelrigg SR, Landreneau RJ, Mack M, et al. Thoracoscopic stapled resection for spontaneous pneumothorax. J Thorac Cardiovasc Surg 1993;105:389-92; discussion 392-3. [PubMed]
- Hatz RA, Kaps MF, Meimarakis G, et al. Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg 2000;70:253-7. [PubMed]
- Sedrakyan A, van der Meulen J, Lewsey J, et al. Video assisted thoracic surgery for treatment of pneumothorax and lung resections: systematic review of randomised clinical trials. BMJ 2004;329:1008. [PubMed]
- Inderbitzi RG, Leiser A, Furrer M, et al. Three years’ experience in video-assisted thoracic surgery (VATS) for spontaneous pneumothorax. J Thorac Cardiovasc Surg 1994;107:1410-5. [PubMed]
- Liu HP, Lin PJ, Hsieh MJ, et al. Thoracoscopic surgery as a routine procedure for spontaneous pneumothorax. Results from 82 patients. Chest 1995;107:559-62. [PubMed]
- Barker A, Maratos EC, Edmonds L, et al. Recurrence rates of video-assisted thoracoscopic versus open surgery in the prevention of recurrent pneumothoraces: a systematic review of randomised and non-randomised trials. Lancet 2007;370:329-35. [PubMed]
- Henry M, Arnold T, Harvey J, et al. BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003;58 Suppl 2:ii39-52. [PubMed]
- Massard G, Thomas P, Wihlm JM. Minimally invasive management for first and recurrent pneumothorax. Ann Thorac Surg 1998;66:592-9. [PubMed]
- Nakanishi K. Long-term effect of a thoracoscopic stapled bullectomy alone for preventing the recurrence of primary spontaneous pneumothorax. Surg Today 2009;39:553-7. [PubMed]
- Horio H, Nomori H, Fuyuno G, et al. Limited axillary thoracotomy vs video-assisted thoracoscopic surgery for spontaneous pneumothorax. Surg Endosc 1998;12:1155-8. [PubMed]
- Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 2005;127:2226-30. [PubMed]
- Cardillo G, Facciolo F, Giunti R, et al. Videothoracoscopic treatment of primary spontaneous pneumothorax: a 6-year experience. Ann Thorac Surg 2000;69:357-61; discussion 361-2. [PubMed]
- Hürtgen M, Linder A, Friedel G, et al. Video-assisted thoracoscopic pleurodesis. A survey conducted by the German Society for Thoracic Surgery. Thorac Cardiovasc Surg 1996;44:199-203. [PubMed]
- Ohno K, Miyoshi S, Minami M, et al. Ipsilateral recurrence frequency after video-assisted thoracoscopic surgery for primary spontaneous pneumothorax. Jpn J Thorac Cardiovasc Surg 2000;48:757-60. [PubMed]
- Ayed AK, Al-Din HJ. The results of thoracoscopic surgery for primary spontaneous pneumothorax. Chest 2000;118:235-8. [PubMed]
- Horio H, Nomori H, Kobayashi R, et al. Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 2002;16:630-4. [PubMed]
- Loubani M, Lynch V. Video assisted thoracoscopic bullectomy and acromycin pleurodesis: an effective treatment for spontaneous pneumothorax. Respir Med 2000;94:888-90. [PubMed]
- Chen JS, Hsu HH, Kuo SW, et al. Effects of additional minocycline pleurodesis after thoracoscopic procedures for primary spontaneous pneumothorax. Chest 2004;125:50-5. [PubMed]
- Cardillo G, Carleo F, Giunti R, et al. Videothoracoscopic talc poudrage in primary spontaneous pneumothorax: a single-institution experience in 861 cases. J Thorac Cardiovasc Surg 2006;131:322-8. [PubMed]
- Sakamoto K, Takei H, Nishii T, et al. Staple line coverage with absorbable mesh after thoracoscopic bullectomy for spontaneous pneumothorax. Surg Endosc 2004;18:478-81. [PubMed]
- Nakanishi K. An apical symphysial technique using a wide absorbable mesh placed on the apex for primary spontaneous pneumothorax. Surg Endosc 2009;23:2515-21. [PubMed]
- Cho S, Ryu KM, Jheon S, et al. Additional mechanical pleurodesis after thoracoscopic wedge resection and covering procedure for primary spontaneous pneumothorax. Surg Endosc 2009;23:986-90. [PubMed]
- Cho S, Huh DM, Kim BH, et al. Staple line covering procedure after thoracoscopic bullectomy for the management of primary spontaneous pneumothorax. Thorac Cardiovasc Surg 2008;56:217-20. [PubMed]
- Muramatsu T, Ohmori K, Shimamura M, et al. Staple line reinforcement with fleece-coated fibrin glue (TachoComb) after thoracoscopic bullectomy for the treatment of spontaneous pneumothorax. Surg Today 2007;37:745-9. [PubMed]
- Baumann MH, Strange C. Treatment of spontaneous pneumothorax: a more aggressive approach? Chest 1997;112:789-804. [PubMed]
- Kawamura M, Sawafuji M, Watanabe M, et al. Frequency of transmission of human parvovirus B19 infection by fibrin sealant used during thoracic surgery. Ann Thorac Surg 2002;73:1098-100. [PubMed]
- Ishida H, Nitanda H, Sakaguchi H, et al. Visceral pleura covered with a polyglycolic acid sheet and autologous blood after thoracoscopic bullectomy for spontaneous pneumothorax. Jpn J Chest Surg 2007;21:645-9.
- Ichihara H, Mine K, Taneda Y, et al. Effects of covering visceral pleura with polyglycolic acid sheet and autologous blood after thoracoscopic bullectomy for spontaneous pneumothorax. Jpn J Chest Surg 2007;21:111-4.
- Ohta S, Hirose M, Ishibashi H. Pleural covering method of polyglycolic acid felt with sodium alginate water solution for prevention of postoperative pulmonary fistula. Kyobu Geka 2008;61:561-3. [PubMed]
- Takei H, Nihi T, Maehara T. Effects of covering visceral pleura with polyglycolic acid felt guided by polydioxanone suture after thoracoscopic bullectomy for spontaneous pneumothorax. Jpn J Chest Surg 2004;18:612-5.