Excessive daytime sleepiness in sleep disorders
Abstract
Excessive daytime sleepiness is a significant public health problem, with prevalence in the community estimated to be as high as 18%. Sleepiness is caused by abnormal sleep quantity or sleep quality. Amongst others, multiple neurological, psychological, cardiac and pulmonary disorders may contribute. Risk factors for excessive sleepiness include obesity, depression, extremes of age and insufficient sleep. In the clinical setting, two of the most commonly encountered causes are obstructive sleep apnoea and periodic limb movement disorder. There is continuing discussion of the mechanisms by which these disorders cause daytime symptoms, with intermittent nocturnal hypoxia, sleep fragmentation and autonomic dysregulation identified as important factors. The increased prevalence of obstructive sleep apnoea in obese subjects does not fully account for the increased rates of daytime sleepiness in this population and there is evidence to suggest that it is caused by metabolic factors and chronic inflammation in obese individuals. Sleepiness is also more common in those reporting symptoms of depression or anxiety disorders and significantly impacts their quality of life. Clinicians should be aware of factors which put their patients at high risk of daytime sleepiness, as it is a debilitating and potentially dangerous symptom with medico-legal implications. Treatment option should address underlying contributors and promote sleep quantity and sleep quality by ensuring good sleep hygiene. However, stimulant medication may be indicated in some cases to allow for more normal daytime functioning.
Key words: Sleep; sleep apnoea; obstructive; nocturnal myoclonus syndrome; obesity; depression
Introduction
Excessive daytime sleepiness (EDS) is the primary concern for many patients presenting with sleep disorder and a significant public health problem. The International Classification of Sleep Disorders (ICSD-2) includes EDS as an essential feature for three diagnostic categories: narcolepsy, hypersomnia and behaviourally induced insufficient sleep syndrome. However, it is also associated with a wide range of diseases, including psychiatric and neurological disorders, pulmonary and cardiac conditions (Table 1). Frequently, there may not be an identifiable cause and the only diagnosis possible is that of idiopathic hypersomnia. However, the most common causes may be found in a disturbance of sleep quality, sleep quantity or other contributors. Most frequently, insufficient sleep duration is responsible for this symptom. This review will give an overview of some of the most common causes of EDS encountered in clinical practice and identify important risk factors for sleepiness in the community.
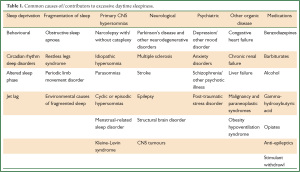
Full table
Prevalence of EDS
The prevalence of self-reported insufficient sleep or excessive daytime sleepiness in the general population has proved difficult to estimate. This is partly due to the lack of a standard definition of EDS, with some studies asking subjects to estimate the severity of their daytime sleepiness, others the number of days per week they experience EDS and others using the Epworth Sleepiness Score (ESS) to assess sleepiness. This score ranges from 0, indicating no daytime sleepiness, to a maximum of 24 (1). The latest “Sleep in America” poll conducted by the American Sleep Foundation found that 18% of respondents scored 10 points or more on the ESS, qualifying them as excessively sleepy (2). Other findings vary significantly. For example, a Japanese study which asked participants “Do you fall asleep when you must not sleep (for example when you are driving a car)?” identified a prevalence of 2.5% (3), whilst a recent Norwegian study in which the ESS was administered over the telephone found that 17.7% of participants had an ESS of 10 or more (4). A US study where EDS was identified based on a moderate or severe rating for the questions “do you feel drowsy or sleepy most of the day but manage to stay awake?” and “do you have any irresistible sleep attacks during the day?” reported a prevalence of 8.7% (5).
EDS is associated with poor performance in the workplace (6) and reduced quality of life with serious economic consequences: a recent Australian study estimated the economic costs of sleepiness at $AUS 4.5 million (approximately £4 million or $4.6 US Dollar), or 0.8% of GDP (7). Importantly, sleepy drivers are at greatly increased risk of involvement in road traffic accidents, which are also more likely to be fatal due to the driver’s failure to brake before impact (8).
Measuring sleepiness
Multiple Sleep Latency Test (MSLT) and ESS
The ESS is the most widely used subjective measure of sleepiness. This takes the form of a questionnaire where patients rate their perceived likelihood of falling asleep in eight everyday situations, to give a score from 0-24 points (1). Although the test is quick and easy to administer, it is dependent on the subject’s interpretation of the rating system. It may be less reliable in very sleepy patients and can be affected by social, cultural and psychological factors such as anxiety or depression, and gender (9,10). The best available objective measure of sleepiness is mean sleep latency, as measured by the MSLT, where patients take successive naps at 2 hour intervals and the time to sleep onset is measured using polysomnographic criteria. Generally, a mean sleep latency of less than 15 minutes is considered being mildly sleepy, less than 10 minutes is moderately and less than 5 minutes qualifies as severely sleepy (11). However, both objective and subjective measures of sleepiness may be confounded by factors such as the patient’s motivation to stay awake (12), sleep hygiene or the previous night’s sleep quality and quantity.
Hypersomnia vs. fatigue
When investigating potential causes of EDS, it is important to distinguish between fatigue and excessive sleepiness, or hypersomnia. Fatigue is, like hypersomnia, a common complaint in general practice; it is a poorly defined feeling of exhaustion or strain associated with many chronic diseases and psychiatric disorders (13). Importantly, severely fatigued patients will not necessarily be sleepy, suggesting that the underlying pathologies are distinct. However, in clinical practice it can be difficult to distinguish between the two and there are recognised cases where fatigue and sleepiness may not be clearly defined (Table 2).
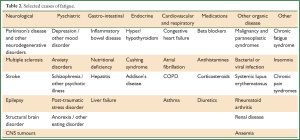
Full table
Causes of EDS
Sleep apnoea and sleep-disordered breathing
The most commonly encountered cause of EDS in a clinical setting is obstructive sleep apnoea (OSA). Sleep apnoea results from total or partial occlusion of the upper airway during sleep, causing apnoeas and hypopnoeas that lead to intermittent hypoxia, arousal from sleep with resulting sleep fragmentation and disturbed sleep architecture. OSA can be reliably diagnosed by using overnight polysomnography studies to assess the number of apnoeas-hypopnoeas per hour of sleep: the apnoea-hypopnoea index (AHI). According to the American Academy of Sleep Medicine criteria, an AHI of 5-15 events per hour represents mild OSA, an AHI of 15-30 as moderate OSA and an AHI>30 as severe. However, this criteria also considers the degree of EDS, which may not correlate with the severity as measured by the AHI. OSA is common worldwide, with the proportion of 30-60 year old adults in the USA with an AHI ≥5 estimated at 24% of men and 9% of women (9). In Europe, estimates of 26% of men and 28% of women with an AHI ≥5 have been reported (14), whilst 9% of Hong Kong males were found to have an AHI ≥5 (15). The percentage of participants with OSA associated with EDS was lower in both the USA study (4% of men and 2% of women) and the Hong Kong study (4% of participants), suggesting that OSA is highly prevalent but often asymptomatic. In the USA, it is estimated that 75-80% of those with symptomatic OSA are undiagnosed, representing a significant population who could benefit from treatment (16).
Patients are rarely aware of night-time disturbance other than snoring, but may complain of excessive sleepiness during the daytime or involuntarily falling asleep. Well recognised risk factors for this condition include an increased BMI, neck circumference, increased age, alcohol use, male gender and anatomical variations which narrow the upper airway.
A hypothesised mechanism for sleep disruption in obesity is that excess tissue around the pharynx narrows the airway, impacting on the critical occlusion pressure of the upper airway (17) and disrupting breathing during sleep. However, this theory has been criticised by a number of authors, who argue that the physical effects of increased fat cannot account for the degree of disruption to breathing.
The factors determining EDS in OSA are not well understood; the severity of OSA measured by AHI does not correlate well with the presence or degree of daytime sleepiness. Early studies found no link with sleep fragmentation and inconsistent results regarding the significance of intermittent nocturnal hypoxaemia (INH) (18,19). However, nasal continuous positive airway pressure (CPAP) to correct INH in OSA, has proved to be an effective treatment for EDS, especially for those with a high AHI or severe sleepiness (20). Colt et al. suggested that this may be due to the correction of sleep fragmentation, rather than the elimination of INH. They studied OSA patients with nasal continuous positive airway pressure (CPAP) treatment to avoid apnoeas and hypopnoeas and correct sleep fragmentation, with or without the induction of INH. INH was induced by the intermittent addition of 100% nitrogen to the air delivered via CPAP. After 2 nights of treatment, there was no significant difference in the change of mean sleep latency in the MSLT observed in each group, leading the authors to suggest that nocturnal hypoxemia was not relevant to the pathogenesis of EDS. However, this study involved only 2 nights of INH and in this short-term design EDS may not significantly change; it is therefore unlikely to be a valid model of the pathological mechanism in OSA. OSA patients experience nocturnal hypoxemia over many years, a chronic process which is thought to cause daytime cognitive dysfunction and damage wake-promoting networks (21) and experience shows that sleep apnoea patients, even when controlled with CPAP therapy, may require weeks or even months of treatment to experience significant changes in their level of sleepiness.
Many studies may have failed to identify clear risk factors for hypersomnolence because they attempted to evaluate a large number of variables in OSA patients with varying degrees of EDS. In a comparison of two groups of OSA patients with either severe EDS {mean [standard deviation, SD] ESS 17 [3] points, MSLT 4 [1] min} or no EDS, {ESS 5 [2] points, MSLT 16 [3] min}, Mediano et al. found that the EDS group had significantly increased sleep efficiency and worse nocturnal intermittent hypoxaemia (22). No significant difference was found in the apnoea-hypopnoea-index (AHI), arousal index or architecture of sleep phases. However, this study failed to control for the possible presence of obesity hypoventilation syndrome (OHS) in the EDS group (23). OHS patients are those who are obese and hypercapnic (PaCO2 >45 mmHg or >6 kPa) without other causes of hypoventilation. In contrast, OSA patients are neither hypoxic nor hypercapnic by day (24). Patients with OHS are known to suffer worse daytime sleepiness than isolated OSA patients matched for age, AHI and body mass index (BMI) (25), potentially confounding the results of Mediano et al. Despite this, the consistent association between nocturnal hypoxaemia and EDS suggests that there may be a linking pathogenic mechanism.
Autonomic arousals during sleep have been discussed as another cause of EDS in patients with sleep-disordered breathing. These arousals involve brainstem nuclei which control sleep and wake cycles as well as cardiac function, leading to autonomic changes without changes to the EEG (26). OSA patients with EDS have an increased ratio of low to high frequency heart rate power (LF/HF) during sleep, a feature which is used to describe vagal and sympathetic tone (27). An elevated LF/HF power ratio indicates an increase in sympathetic output to the heart, possibly caused by repeated autonomic arousals. The significance of the LF/HF power ratio remains when OHS patients are excluded, whilst no difference in AHI and nocturnal hypoxaemia is found between patients with or without EDS (28). This evidence suggests that lower oxygenation and increased sympathetic cardiac tone during sleep are key factors contributing to EDS in patients with sleep-disordered breathing.
Periodic Limb Movement Disorder (PLMD) and Restless Legs Syndrome (RLS)
Periodic limb movement disorder (PLMD) is another commonly-encountered sleep disorder and potentially a cause of daytime sleepiness. It was initially identified in patients with RLS, with approximately 80% of RLS patients undergoing polysomnography found to have PLMD (29). However, PLMD is recognised as a separate condition from RLS (11). PLMD patients experience involuntary, but non-epileptic, stereotypical movements of their limbs, especially during non-rapid eye movement (NREM) sleep and during the 1st half of the night (30). Up to 25% of those presenting with other sleep disorders, such as OSA, rapid eye movement (REM) sleep behaviour disorder or narcolepsy may also suffer from PLMD (31) which, in part, explains the difficulties in understanding the effects of isolated PLMD. PLMD is commonly thought to be under-diagnosed, with prevalence in the community estimated at 3.9% (32). Several studies have suggested a role for dysregulation of dopaminergic transmission in the pathogenesis of PLMD, supported by the observation that dopamine agonists can be an effective treatment (33).
Recent work to establish the cause of EDS in PLMD has focused on the presence of autonomic arousals seen in this disorder. It is not obvious whether PLMs cause the arousals or are a reflection of altered autonomic function, although the periodic nature of movements in PLMD has led to comparisons with the “cyclic alternating pattern” (CAP) sometimes visible on the EEG and used as a marker of arousal instability during sleep (34). This pattern consists of the background EEG pattern (phase B) interspersed with bursts of delta wave activity (phase A). In 1996, Parrino et al. demonstrated that PLMs are mostly present during periods of CAP, and that there are increased limb movements during phase A activity. Ferrillo has suggested that this signifies that cortical arousals in PLMD are synchronised with a brainstem network regulating cardiovascular and respiratory changes, an arrangement which also underlies the CAP (35).
More recently, polysomnographic data from PLMD patients was used to examine the temporal relationship between changes in the EEG, heart rate and limb movements in both REM and NREM sleep. A number of studies have detected autonomic activation several seconds before either limb movement or EEG changes, suggesting that sympathetic activation leads to sub-cortical activation and facilitation of both cortical arousal and PLM (36). This, similarly to patients with sleep-disordered breathing, implies that sympathetic over-activity and not the PLMs may be the cause of sleep disruption, resulting in EDS.
EDS in the general population
Outside of the clinical setting, EDS is a widespread problem in the community, with estimated prevalence as high as 18% (2). A number of factors contribute to EDS and this may range from chronic insufficient sleep to poor sleep hygiene, use of modern media in bed and female gender. However, it can be difficult to identify significant risk factors. Interviews with 1997 16-93 year olds in the UK, carried out by Groeger et al., found that 18% of subjects reported insufficient sleep on most nights; 58% of participants had suffered sleep problems on at least one night during the previous week (37), which was similar to the US sleep survey findings (2). However, only 5% of respondents reported sleeping less than 5 hours a night, with little gender difference in self-reported sleep duration (37).
The importance of long-term sleep insufficiency is unclear. Bonnet and Arand have argued that even small reductions of sleep time may have significant effects on the mean sleep latency and that reduced awareness due to sleepiness should be a serious public health concern (38). A study showed that loss of two hours of sleep can cause a 32% reduction in MSL (39). However, there is conflicting evidence, including animal studies, indicating that sleep times extend beyond those required if there are few incentives to stay awake, and this may have serious implications considering the social background of subjects and potential associations with underlying depression. Additionally, normal subjects will sleep for longer than usual in the right environment, even when EDS is not detected in the MSLT (40), suggesting that sleep times alone are of little use in estimating the severity of sleep disorders in the community.
Obesity and EDS
Obesity is a factor consistently linked to daytime sleepiness (41), with obese subjects twice as likely to report EDS than non-obese individuals (5). Whilst the increased prevalence of OSA in obese subjects may account for some of this difference, obesity is associated with hypersomnolence even in the absence of sleep-disordered breathing (5,42,43). The reasons for this are not fully understood, although a number of factors have been shown to be predictive of EDS in obese patients, suggesting that the underlying mechanism is multifactorial.
Perhaps unexpectedly, a study of obese patients presenting for bariatric surgery found that AHI is not predictive of daytime sleepiness (44), suggesting that other factors may be more important than the presence of OSA. A recent cross-sectional study of OSA patients also found that obesity and depressive symptoms, but not AHI, were predictive of EDS (45). Even snoring has been found to be a predictor of sleepiness independently of AHI and other sleep parameters (46). The importance of factors other than sleep disordered breathing could also explain why CPAP therapy sometimes fails to correct EDS, especially in those with mild OSA (20).
Metabolic disruption and chronic inflammation in obesity may be more relevant to EDS than the mechanical effects of excess weight. This hypothesis may be underlined by the fact that adipose tissue is the largest endocrine organ, producing multiple adipokines. Vgontzas and colleagues have suggested that daytime sleepiness in obesity is a manifestation of a metabolic abnormality leading to hyperarousal at night and hypoarousal during the day. This was based on their observations that obese subjects have shorter sleep latencies and maintain sleep more effectively during the day, but have difficulty falling asleep and maintaining sleep at night. They also identified differences in sleep architecture, with obese patients experiencing more REM sleep in the early hours and less REM sleep in the later part of the night compared to controls. This latter point could indicate a circadian shift of REM sleep in the obese. In addition, levels of insulin and pro-inflammatory cytokines such as interleukin-6, tumour necrosis factor alpha (TNF-α) are increased in the obese, supporting the hypothesis that obesity is a chronic inflammatory state.
Vgontzas’s group examined whether these metabolic disturbances directly cause hypersomnolence by trialling the use of etanercept, an anti-TNF drug, to treat EDS in obese patients with OSA over three weeks. The mean sleep latency of the treatment group increased by 3.1 (1.0) min in the MSLT (P<0.05) (47), but, although this is a statistically significant result, this study involved only eight patients and larger-scale studies may be needed to provide further understanding of the efficacy of such medical treatment.
Depression and EDS
In both obese and non-obese subjects, depression is strongly associated with sleepiness. However, 70% of those with depressive disorder complain of difficulty initiating and maintaining sleep and, thus, insomnia and fatigue rather than daytime sleepiness are often regarded as the most important problems, with a number of studies confirming the importance of insomnia as an independent predictor of suicidal ideation and behaviour (48,49). Most clinical rating scales for depression enquire about fatigue and tiredness rather than EDS specifically, so the significance of sleepiness in depression may be underestimated (50). Daytime sleepiness has been shown to correlate with increased depression tendency scores in the general public (51) and, in addition, patients with OSA have high rates of depressive disorders (15-56% of patients vs. 6-7% of the healthy population) (52,53).
Examination of the link between sleepiness and depression is further complicated by the fact that both are influenced by other factors such as medication, comorbid systemic disease, alcohol use and anxiety. One approach to further understand these interactions has been to explore the role of genetic factors; both depression and daytime sleepiness are moderately associated with heritability (coefficients between 38-48% for EDS (54,55) and 16-55% for depression (56,57). A large number of genes show an association with depression, especially within the serotonergic system (58,59), but only a small number of gene association studies for EDS has been completed. A cross sectional study of elderly twins found a significant genetic correlation of 0.4, suggesting the presence of genes which affect both conditions (50). Association of EDS has been found with variations in the orexin/hypocretin gene OC2R (60), and in narcoleptic patients with the catechol-O-methyltransferase (COMT) gene necessary for degradation of dopamine (61).
Age and EDS
The prevalence of EDS also changes with age, with a number of studies finding increased EDS in the very young and very old. Prevalence of EDS decreases in those over 35 year olds, and increases again in the over 75 year olds range (5). EDS in the young is most likely due to insufficient sleep, whilst sleepiness in the old is more commonly associated with health problems such as diabetes and cardiovascular disease. Additionally, both sleep efficiency and sleepiness become less common in middle age, suggesting that EDS in older people is not solely due to less efficient sleep, but may also hint at changes in the everyday routines that working life demands. Another suggested mechanism is that hormonal sleep homeostasis is disrupted in older people. This is supported by the observation that administration of an arousal-promoting hormone, such as corticotrophin-releasing hormone, at the beginning of sleep causes more sleep disturbance in older subjects than younger (62).
Other risk factors for EDS
Cross-sectional studies have proved useful in identifying other risk factors for EDS in the general population, including shift-work, poor sleep hygiene (e.g., using mobile phones before bedtime) and loneliness (63,64). Shift work sleep syndrome, a type of circadian rhythm disorder in which patients have difficulty falling asleep and waking up, is a well recognised cause of EDS (65) estimated to affect about 10% of those who work irregular hours (66). Working outside of daylight hours disrupts the circadian sleep-wake cycle and decreases both the duration and efficiency of sleep (67). A recent study of over 3,000 people found that night workers were 2.7 times more likely than day workers to feel moderately to severely sleepy at work (68). Additionally, sleepiness is a commonly encountered symptom in serious systemic disease. Examples include cardiac failure, respiratory illness (e.g., COPD), malignancy and a range of neurological conditions (69-73).
Medication
People suffering from EDS may self-medicate or use caffeine, exacerbating the problem. Caffeine increases sleep latency and reduces both total sleep time and the percentage of stage 4 sleep (74). These effects are most likely due to its antagonism of the A1 and A2A adenosine receptors distributed widely throughout the central nervous system (CNS) (75,76). Adenosine is known to inhibit cholinergic neurons located in the basal forebrain which are involved in arousal, so caffeine may promote wakefulness by disinhibiting this system (77). However, it is difficult to assess the impact of caffeine in the population due to the wide variety of caffeine sources and the inconsistency of caffeine intake. A British population-based study found that high consumption (>6 cups of tea or coffee per day) was associated with higher rates of severe sleepiness (78) compared to moderate caffeine intake. However, it remains unclear to what extent lifestyle issues may contribute to these results. Therefore, lifestyle adjustment and sufficient sleep quantity and quality (sleep hygiene) should be at the centre of therapeutic efforts, but if such measures are insufficient adjunct stimulant therapy (e.g., modafinil) may be used.
Summary
Daytime sleepiness is a common, debilitating and potentially dangerous symptom, which is likely to be under-recognised. It can be caused by multiple contributors, usually interfering with sleep quantity and sleep quality (Table 3). Patients with OSA often, but not invariably, suffer from hypersomnolence as a result of poor nocturnal oxygenation and dysregulation of autonomic function. It is thought that these factors damage neural networks involved in wake promotion and disrupt sleep through autonomic arousals. In PLMD, the finding that autonomic changes precede the cortical activation causing leg movement suggests that an underlying disorder of autonomic regulation leads to disrupted sleep. Additionally, clinicians should be aware of factors which put their patients at high risk of EDS, including shift work, obesity, depressive symptoms and poor sleep hygiene. Of these, further investigation of the hypothesised mechanisms by which obesity may cause EDS are of particular interest, due to the widespread prevalence of both of these conditions. Treatment should always focus on the underlying cause, promoting appropriate sleep quantity and quality by establishing good sleep hygiene. Available stimulant therapy may be used as adjunct in certain cases. To optimise treatment of patients with EDS, it will be important to consider the wide range of unidentified risk factors which may be contributing to this symptom.
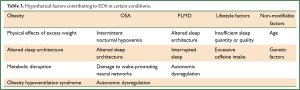
Full table
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnoea. The Epworth Sleepiness Scale. Chest 1993;103:30-6.
- Swanson LM, Arnedt JT, Rosekind MR, et al. Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res 2011;20:487-94.
- Kaneita Y, Ohida T, Uchiyama M, et al. Excessive daytime sleepiness among the Japanese general population. J Epidemiol 2005;15:1-8.
- Pallesen S, Nordhus IH, Omvik S, et al. Prevalence and risk factors of subjective sleepiness in the general adult population. Sleep 2007;30:619-24.
- Bixler EO, Vgontzas AN, Lin HM, et al. Excessive daytime sleepiness in a general population sample: the role of sleep apnoea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 2005;90:4510-5.
- Haavisto ML, Porkka-Heiskanen T, Hublin C, et al. Sleep restriction for the duration of a work week impairs multitasking performance. J Sleep Res 2010;19:444-54.
- Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep 2006;29:299-305.
- Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ 2002;324:1125.
- Chervin RD, Aldrich MS. The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnoea. Neurology 1999;52:125-31.
- Olson LG, Cole MF, Ambrogetti A. Correlations among Epworth Sleepiness Scale scores, multiple sleep latency tests and psychological symptoms. J Sleep Res 1998;7:248-53.
- American Academy of Sleep Medicine. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago, Illinois: American Academy of Sleep Medicine, 2001.
- Bonnet MH, Arand DL. Impact of motivation on Multiple Sleep Latency Test and Maintenance of Wakefulness Test measurements. J Clin Sleep Med 2005;1:386-90.
- Lewis G, Wessely S. The epidemiology of fatigue: more questions than answers. J Epidemiol Community Health 1992;46:92-7.
- Durán J, Esnaola S, Rubio R, et al. Obstructive sleep apnoea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med 2001;163:685-9.
- Ip MS, Lam B, Lauder IJ, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest 2001;119:62-9.
- Young T, Evans L, Finn L, et al. Estimation of the clinically diagnosed proportion of sleep apnoea syndrome in middle-aged men and women. Sleep 1997;20:705-6.
- Isono S. Obesity and obstructive sleep apnoea: mechanisms for increased collapsibility of the passive pharyngeal airway. Respirology 2012;17:32-42.
- Guilleminault C, Partinen M, Quera-Salva MA, et al. Determinants of daytime sleepiness in obstructive sleep apnoea. Chest 1988;94:32-7.
- Bédard MA, Montplaisir J, Richer F, et al. Nocturnal hypoxemia as a determinant of vigilance impairment in sleep apnoea syndrome. Chest 1991;100:367-70.
- Patel SR, White DP, Malhotra A, et al. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnoea: results of a meta-analysis. Arch Intern Med 2003;163:565-71.
- Row BW. Intermittent hypoxia and cognitive function: implications from chronic animal models. Adv Exp Med Biol 2007;618:51-67.
- Mediano O, Barcelo A, de la Pena M, et al. Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur Respir J 2007;30:110-3.
- BaHammam A. Excessive daytime sleepiness in patients with sleep-disordered breathing. Eur Respir J 2008;31:685-6.
- Rapoport DM, Garay SM, Epstein H, et al. Hypercapnia in the obstructive sleep apnoea syndrome. A reevaluation of the “Pickwickian syndrome”. Chest 1986;89:627-35.
- Hida W, Okabe S, Tatsumi K, et al. Nasal continuous positive airway pressure improves quality of life in obesity hypoventilation syndrome. Sleep Breath 2003;7:3-12.
- Bonsignore MR, Parati G, Insalaco G, et al. Baroreflex control of heart rate during sleep in severe obstructive sleep apnoea: effects of acute CPAP. Eur Respir J 2006;27:128-35.
- Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 1996;17:354-81.
- Castiglioni P, Lombardi C, Di Rienzo M, et al. What are the causes of excessive daytime sleepiness in patients with sleep-disordered breathing? Eur Respir J 2008;32:526-7.
- Comella CL. Restless legs syndrome: treatment with dopaminergic agents. Neurology 2002;58:S87-92.
- Coleman RM, Pollak CP, Weitzman ED. Periodic movements in sleep (nocturnal myoclonus): relation to sleep disorders. Ann Neurol 1980;8:416-21.
- Karatas M. Restless legs syndrome and periodic limb movements during sleep: diagnosis and treatment. Neurologist 2007;13:294-301.
- Ohayon MM, Roth T. Prevalence of restless legs syndrome and periodic limb movement disorder in the general population. J Psychosom Res 2002;53:547-54.
- Manconi M, Ferri R, Zucconi M, et al. Preferential D2 or preferential D3 dopamine agonists in restless legs syndrome. Neurology 2011;77:110-7.
- Terzano MG, Parrino L, Rosa A, et al. CAP and arousals in the structural development of sleep: an integrative perspective. Sleep Med 2002;3:221-9.
- Ferrillo F, Beelke M, Canovaro P, et al. Changes in cerebral and autonomic activity heralding periodic limb movements in sleep. Sleep Med 2004;5:407-12.
- Guggisberg AG, Hess CW, Mathis J. The significance of the sympathetic nervous system in the pathophysiology of periodic leg movements in sleep. Sleep 2007;30:755-66.
- Groeger JA, Zijlstra FR, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J Sleep Res 2004;13:359-71.
- Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep 1995;18:908-11.
- Rosenthal L, Roehrs TA, Roehrs T, et al. Level of sleepiness and total sleep time following various time in bed conditions. Sleep 1993;16:226-32.
- Harrison Y, Horne JA. Should we be taking more sleep? Sleep 1995;18:901-7.
- Steier J, Jolley CJ, Jolley CJ, et al. Neural respiratory drive in obesity. Thorax 2009;64:719-25.
- Vgontzas AN, Tan TL, Bixler EO, et al. Sleep apnoea and sleep disruption in obese patients. Arch Intern Med 1994;154:1705-11.
- Resta O, Foschino Barbaro MP, Bonfitto P, et al. Low sleep quality and daytime sleepiness in obese patients without obstructive sleep apnoea syndrome. J Intern Med 2003;253:536-43.
- Dixon JB, Dixon ME, Anderson ML et al. Daytime sleepiness in the obese: not as simple as obstructive sleep apnoea. Obesity 2007;15:2504-11.
- Pamidi S, Knutson KL, Ghods F, et al. Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnoea: Cross-sectional analysis of a large clinical population. Sleep Med 2011;12:827-31.
- Svensson M, Franklin KA, Theorell-Haglow J, et al. Daytime sleepiness relates to snoring independent of the apnoea-hypopnea index in women from the general population. Chest 2008;134:919-24.
- Vgontzas AN, Zoumakis E, Lin HM, et al. Marked decrease in sleepiness in patients with sleep apnoea by etanercept, a tumor necrosis factor-alpha antagonist. J Clin Endocrinol Metab 2004;89:4409-13.
- McCall WV, Blocker JN, D'Agostino R Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med 2010;11:822-7.
- Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord 2012;136:743-50.
- Lessov-Schlaggar CN, Bliwise DL, Krasnow RE, et al. Genetic association of daytime sleepiness and depressive symptoms in elderly men. Sleep 2008;31:1111-7.
- Regestein Q, Natarajan V, Pavlova M, et al. Sleep debt and depression in female college students. Psychiatry Res 2010;176:34-9.
- Sharafkhaneh A, Giray N, Richardson P, et al. Association of psychiatric disorders and sleep apnoea in a large cohort. Sleep 2005;28:1405-11.
- Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry 2003;54:216-26.
- Carmelli D, Bliwise DL, Swan GE, et al. A genetic analysis of the Epworth Sleepiness Scale in 1560 World War II male veteran twins in the NAS-NRC Twin Registry. J Sleep Res 2001;10:53-8.
- Desai AV, Cherkas LF, Spector TD, et al. Genetic influences in self-reported symptoms of obstructive sleep apnoea and restless legs: a twin study. Twin Res 2004;7:589-95.
- Kendler KS, Walters EE, Truett KR, et al. Sources of individual differences in depressive symptoms: analysis of two samples of twins and their families. Am J Psychiatry 1994;151:1605-14.
- Jang KL, Livesley WJ, Taylor S, et al. Heritability of individual depressive symptoms. J Affect Disord 2004;80:125-33.
- Middeldorp CM, Slof-Op’t Landt MC, Medland SE, et al. Anxiety and depression in children and adults: influence of serotonergic and neurotrophic genes? Genes Brain Behav 2010;9:808-16.
- Wray NR, Pergadia ML, Blackwood DH, et al. Genome-wide association study of major depressive disorder: new results, meta-analysis, and lessons learned. Mol Psychiatry 2012;17:36-48.
- Thompson MD, Comings DE, Abu-Ghazalah R, et al. Variants of the orexin2/hcrt2 receptor gene identified in patients with excessive daytime sleepiness and patients with Tourette’s syndrome comorbidity. Am J Med Genet B Neuropsychiatr Genet 2004;129B:69-75.
- Dauvilliers Y, Neidhart E, Lecendreux M, et al. MAO-A and COMT polymorphisms and gene effects in narcolepsy. Mol Psychiatry 2001;6:367-72.
- Vgontzas AN, Bixler EO, Wittman AM, et al. Middle-aged men show higher sensitivity of sleep to the arousing effects of corticotropin-releasing hormone than young men: clinical implications. J Clin Endocrinol Metab 2001;86:1489-95.
- Kim H, Young T. Subjective daytime sleepiness: dimensions and correlates in the general population. Sleep 2005;28:625-34.
- Kurina LM, Knutson KL, Hawkley LC, et al. Loneliness is associated with sleep fragmentation in a communal society. Sleep 2011;34:1519-26.
- Thorpy M. Understanding and diagnosing shift work disorder. Postgrad Med 2011;123:96-105.
- Drake CL, Roehrs T, Richardson G, et al. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004;27:1453-62.
- Folkard S. Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm. Chronobiol Int 2008;25:215-24.
- Ohayon MM, Smolensky MH, Roth T. Consequences of shiftworking on sleep duration, sleepiness, and sleep attacks. Chronobiol Int 2010;27:575-89.
- Riegel B, Ratcliffe SJ, Sayers SL, et al. Determinants of excessive daytime sleepiness and fatigue in adults with heart failure. Clin Nurs Res 2012;21:271-93.
- Karachaliou F, Kostikas K, Pastaka C, et al. Prevalence of sleep-related symptoms in a primary care population - their relation to asthma and COPD. Prim Care Respir J 2007;16:222-8.
- Gibbins J, McCoubrie R, Kendrick AH, et al. Sleep-wake disturbances in patients with advanced cancer and their family carers. J Pain Symptom Manage 2009;38:860-70.
- Baumann CR, Werth E, Stocker R, et al. Sleep-wake disturbances 6 months after traumatic brain injury: a prospective study. Brain 2007;130:1873-83.
- Diederich NJ, McIntyre DJ. Sleep disorders in Parkinson's disease: Many causes, few therapeutic options. J Neurol Sci 2012;314:12-9.
- Lasagna L. Dose-related sleep disturbances induced by coffee and caffeine. Clin Pharmacol Ther 1977;21:244.
- Mazzotti DR, Guindalini C, Pellegrino R, et al. Effects of the adenosine deaminase polymorphism and caffeine intake on sleep parameters in a large population sample. Sleep 2011;34:399-402.
- Huang ZL, Urade Y, Hayaishi O. The role of adenosine in the regulation of sleep. Curr Top Med Chem. 2011;11:1047-57.
- Basheer R, Strecker RE, Thakkar MM, et al. Adenosine and sleep-wake regulation. Prog Neurobiol 2004;73:379-96.
- Ohayon MM, Caulet M, Philip P, et al. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med 1997;157:2645-52.


