Etomidate in sepsis: understanding the dilemma
Etomidate is the most commonly utilized induction agent for rapid sequence intubation in emergency departments in the United States (1). Favorable characteristics include reliably good intubating conditions, a rapid onset and offset of activity, non-renal elimination, and maintenance of the cardiorespiratory drive (2). Unfortunately, etomidate causes relative adrenal insufficiency in up to 90% of patients after a single dose (3). Serious safety concerns first surfaced in the early 1980’s when continuous infusions were associated with increased mortality in trauma patients (4,5). Since then, there has been considerable uncertainty regarding its role for rapid sequence intubation, especially in septic patients who may depend on their adrenal reserves for survival during the acute phase of illness (6,7). Understanding the history of this controversy, and reviewing the most recent research into etomidate use in sepsis may help clinicians decide whether or not to use the drug in routine clinical practice.
Adrenal insufficiency and mortality in sepsis
Cortisol is the most abundant endogenous glucocorticoid. Physiologically, it increases vascular responsiveness to catecholamines and angiotensin II, and has anti-inflammatory effects (8). An association between adrenal function and clinical outcomes in septic patients was first proposed in the early 1900’s (9). Ambiguity in the definition of adrenal insufficiency has led to conflicting results regarding its clinical significance for nearly 100 years. Despite this, several studies have confirmed that a baseline cortisol <10 mcg/mL or failure to increase cortisol levels by >9 mcg/dL after adrenocorticotropin challenge portends a poor outcome for patients with sepsis (10-12). Based on these findings, it is generally accepted that adrenal insufficiency is associated with increased mortality in sepsis.
Single-dose etomidate and adrenal insufficiency in critical illness
Etomidate-induced adrenal insufficiency was first suggested in the early 1980’s (4); a subsequent study including rat adrenal cells confirmed that etomidate administration inhibited adrenal function (13). More specifically, etomidate blocks cytochrome 11B1 (11β-hydroxylase), 11B2, and 11A, reducing the conversion of cholesterol to cortisol (14). This synthetic pathway is responsible for approximately 80% of circulating cortisol (8). Studies of mixed cohorts of critically ill patients have shown that the inhibitory effects of etomidate on adrenal function are most pronounced 4-24 hours after a dose, but inhibition can last for up to 72 hours (14-16). Several meta-analyses have confirmed an association between single-dose etomidate and adrenal insufficiency; however the actual duration of inhibition and relevance in septic patients remains poorly defined (17-19).
Etomidate-induced adrenal insufficiency and outcomes in sepsis
An association between etomidate and clinical outcomes has been debated for several years, and prompted to completion several meta-analyses (Table 1). The first found an association of etomidate and increased mortality when studies including septic patients were analyzed [RR 1.22 (95% CI: 1.11-1.35), P<0.0001, I2=74%] (17). In that analysis, randomized and non-randomized studies were combined and there was significant heterogeneity of the results (20). A year later, a second meta-analysis again found etomidate was associated with increased mortality in septic patients in a pooled analysis [RR 1.20 (95% CI: 1.02-1.42), no P value given, I2=4.9%]. In a sensitivity analysis of randomized-controlled trials, the investigators also found the use of etomidate to be associated with increased mortality [RR 1.26 (1.06-1.50), no P value given, I2=11.6%] (18). These findings have been criticized because data presented as being from randomized-controlled trials were in fact derived from secondary post-hoc analyses in trials evaluating other agents (21).
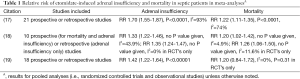
Full table
A more recent meta-analysis of etomidate use in sepsis importantly updates these older efforts with a more rigorous and complete analysis. Among two pooled prospective randomized trials that included septic patients, Gu and colleagues demonstrated a lack of association of etomidate administration and mortality [RR 1.20 (95% CI: 0.84-1.72), P=0.31, I2=0%]. Their subsequent analysis of 16 observational studies confirmed this finding [RR 1.05 (95% CI: 0.97-1.13), P=0.23, I2=25%] (19). These results, involving 5,552 patients in total, agree with the largest retrospective cohort study published to date (n=2014), which found that etomidate administration to patients with sepsis was not associated with hospital mortality (37.2% vs. 37.8%, P=0.77), ICU mortality (30.1% vs. 30.2%, P=0.99), hospital or ICU length of stay, duration of mechanical ventilation, or post-intubation vasopressor days. A secondary analysis in that study limited to patients with septic shock also showed no association of etomidate use and outcome (22).
The meta-analysis by Gu et al. is the most intensive of etomidate use in sepsis to date, and the authors should be commended for their work (19). Nonetheless, the findings must be interpreted with caution. Only two randomized controlled trials were included yielding 196 patients (n=102 received etomidate). One of these studies analyzed the effect of etomidate in a non-stratified subgroup of septic patients, which represented only 16% of the study population (23). In the meta-analysis of observational studies, the McPhee article reflects 17% of the weight of the meta-analysis (19). Additionally, the comparator induction agent was unknown in 15 of the 16 (94%) observational studies. Similarly, the authors were unable to assess secondary outcomes (i.e., hospital or ICU length of stay and duration of mechanical ventilation) due to poor reporting in the source data. So, as in all meta-analyses, the findings by Gu et al. are limited by the quality of the studies available (19).
Should etomidate be used as an induction agent in septic patients?
The most rigorous meta-analysis suggests that etomidate can be safely used in septic patients (19). Ketamine is an attractive alternative in patients with sepsis as it does not depress cardiorespiratory drive, has a rapid onset of action, and has been shown to be non-inferior to etomidate in critically ill patients when co-administered with succinylcholine and infusions of midazolam and an opioid analgesic (23). Development of novel induction agents may also help resolve this clinical conundrum. Carboetomidate contains a five-membered pyrrole ring rather than an imidazole ring and is three times less potent than etomidate as an adrenal suppressant. Cyclopropyl-methoxycarbonyl etomidate and methoxycarbonyl carboetomidate represent other investigational analogs that are up to 300 times less potent inhibitors of adrenal function (24).
Although there is inadequate evidence to justify removing etomidate from clinical use as an induction agent, and the most current meta-analysis supports its use, we believe that the question of etomidate’s safety has not been definitively answered. Clinicians must weigh the pros and cons of etomidate administration in a given patient, and determine on an individual basis if its administration is warranted. This uncertainty will remain until definitive data are developed.
Acknowledgements
The authors thank the editors of the Journal of Thoracic Disease for the opportunity to contribute.
Footnote
Provenance: This is a Guest Editorial commissioned by the Section Editor Wan-Jie Gu (Department of Anesthesiology, Affiliated Drum Tower Hospital, Medical College of Nanjing University, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sagarin MJ, Barton ED, Chng YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med 2005;46:328-36. [PubMed]
- Hampton JP. Rapid-sequence intubation and the role of the emergency department pharmacist. Am J Health Syst Pharm 2011;68:1320-30. [PubMed]
- Mokhlesi B. Corticosteroids for patients with septic shock. JAMA 2003;289:43-author reply 43-4. [PubMed]
- Watkins J. Potential hazards of prolonged anaesthesia with etomidate and althesin. Lancet 1983;1:1434-5. [PubMed]
- Watt I, Ledingham IM. Mortality amongst multiple trauma patients admitted to an intensive therapy unit. Anaesthesia 1984;39:973-81. [PubMed]
- Hunter BR, Kirschner J. In patients with severe sepsis, does a single dose of etomidate to facilitate intubation increase mortality? Ann Emerg Med 2013;61:571-2. [PubMed]
- Lauzier F, Turgeon AF. Etomidate: buy now, pay later?*. Crit Care Med 2012;40:3086-7. [PubMed]
- Marik PE, Pastores SM, Annane D, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med 2008;36:1937-49. [PubMed]
- Waterhouse R. A case of suprarenal apoplexy. Lancet 1911;1:577-8.
- Rothwell PM, Udwadia ZF, Lawler PG. Cortisol response to corticotropin and survival in septic shock. Lancet 1991;337:582-3. [PubMed]
- Annane D, Maxime V, Ibrahim F, et al. Diagnosis of adrenal insufficiency in severe sepsis and septic shock. Am J Respir Crit Care Med 2006;174:1319-26. [PubMed]
- Annane D, Sébille V, Troché G, et al. A 3-level prognostic classification in septic shock based on cortisol levels and cortisol response to corticotropin. JAMA 2000;283:1038-45. [PubMed]
- Wagner RL, White PF, Kan PB, et al. Inhibition of adrenal steroidogenesis by the anesthetic etomidate. N Engl J Med 1984;310:1415-21. [PubMed]
- den Brinker M, Hokken-Koelega AC, Hazelzet JA, et al. One single dose of etomidate negatively influences adrenocortical performance for at least 24h in children with meningococcal sepsis. Intensive Care Med 2008;34:163-8. [PubMed]
- Vinclair M, Broux C, Faure P, et al. Duration of adrenal inhibition following a single dose of etomidate in critically ill patients. Intensive Care Med 2008;34:714-9. [PubMed]
- Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med 2001;8:1-7. [PubMed]
- Albert SG, Ariyan S, Rather A. The effect of etomidate on adrenal function in critical illness: a systematic review. Intensive Care Med 2011;37:901-10. [PubMed]
- Chan CM, Mitchell AL, Shorr AF. Etomidate is associated with mortality and adrenal insufficiency in sepsis: a meta-analysis*. Crit Care Med 2012;40:2945-53. [PubMed]
- Gu WJ, Wang F, Tang L, et al. Single-dose etomidate does not increase mortality in patients with sepsis: a systematic review and meta-analysis of randomized controlled trials and observational studies. Chest 2015;147:335-46. [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [PubMed]
- Sterling SA, Puskarich MA, Jones AE. The effect of etomidate on mortality in sepsis remains unclear. Crit Care Med 2013;41:e95. [PubMed]
- McPhee LC, Badawi O, Fraser GL, et al. Single-dose etomidate is not associated with increased mortality in ICU patients with sepsis: analysis of a large electronic ICU database. Crit Care Med 2013;41:774-83. [PubMed]
- Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet 2009;374:293-300. [PubMed]
- Gin T. Hypnotic and sedative drugs--anything new on the horizon? Curr Opin Anaesthesiol 2013;26:409-13. [PubMed]


