Subxiphoid uniportal thoracoscopic extended thymectomy
Introduction
Uniportal video-assisted thoracic surgery (VATS) has become a sophisticated technique capable of handling some of the most intricate and difficult thoracic operations. The potential advantages of fewer surgical incisions, better cosmesis, less post-operative pain and fewer paraesthesias have made the technique increasingly popular around the world. We report here our first six consecutive experience in performing thoracoscopic extended thymectomy through a single subxiphoid incision.
Case series
Between October 2014 to February 2015, six patients (one male) with thymic diseases received subxiphoid uniportal thoracoscopic extended thymectomy. All the operations were conducted by the same surgical team. Mean age was 50.5±13.1 years (range, 26-62 years). Mean BMI was 26.0±4.5 (range, 23.9-32.4). Mean diameter of the thymic lesion was 3.3±0.8 cm (range, 2-4 cm).
Operative techniques
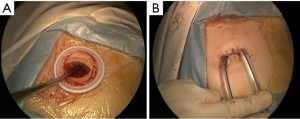
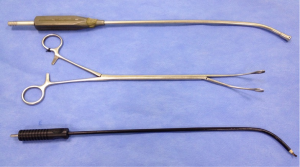
Under general anesthesia with selective one lung ventilation, the patient was placed in the supine position with a roll placed beneath the thoracic spine to elevate the thoracic cage. A 3 to 4 cm transverse incision was made just above the xiphoid process. After removal of the xiphoid process, a midline retrosternal tunnel was created by blunt finger dissection, and a wound protector was placed to provide optimal exposure (Figure 1). A 10-mm, 30 degree angled thoracoscope was used during the operation. Most dissection was performed by an endoscopic electrocautery and a long curved ring forceps. An angled suction tube was introduced for smoke evacuation and exposure of surgical field (Figure 2).
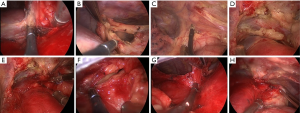
Firstly, the right pleural cavity was opened during left lung ventilation (Figure 3A), the right pericardial and epiphrenic fat pads were dissected from the pericardium and diaphragm with electrocautery (Figure 3B). The right lobe of thymus and mediastinal fat tissues anterior to the phrenic nerve was dissected from the pericardium and ascending aorta by moving cephalically (Figure 3C). With careful and meticulous dissection, the conjunction of the innominate vein and superior vena cava was clearly visualized (Figure 3D). The right superior thymic horn was dissected and pulled to the left side by ring forceps, facilitating separation of the gland from the underlying innominate vein. The course of the innominate vein was traced to identify all the thymic veins. Usually, two to four thymic veins draining into the left innominate vein were identified and ligated by LigaSure device (Figure 3E). Secondly, the left mediastinal pleura was divided during right lung ventilation (Figure 3F), the left pericardial fat was dissected from the pericardium (Figure 3G), and the adipose tissue was dissected from the aorta-pulmonary window space by moving cephalically (Figure 3H). Left superior thymic horn was also dissected completely. Finally, the totally freed thymus gland and mediastinal fat tissue could be brought out from the subxiphoid incision. A 28-Fr thoracic tube was inserted into each side of the pleural cavity through the incision and secured to the chest wall. Ventilation of both lungs was resumed. The incision was closed in a standard manner. Generally, the patient was extubated immediately after the operation. The thoracic tubes were usually removed on the 3rd to 4th postoperative day, and the patients were discharged the following day.
Results
The mean operative time was 155±55 minutes (range, 90-240 minutes). The mean intraoperative blood loss was 78.3±47.1 mL (range, 20-150 mL). There was no conversion to sternotomy. The mean postoperative hospital stay was 4.5±2.3 days (range, 3-9 days). Except for one patient who needed prolonged mechanical ventilatory support, there were no other perioperative complications or mortalities. All of the subxiphoid wounds healed well. The postoperative diagnosis of the six cases was as follows: Masaoka stage I thymoma in three cases (Type B2 Thymoma in two patients, Type AB Thymoma in one patient), thymic cyst in two cases (one unilocular and one multilocular thymic cyst), and true thymic hyperplasia in one patient.
Comments
Median sternotomy, partial or full, remained the gold standard for thymectomy. With recent advances in thoracoscopic instrumentation and techniques, VATS has become a viable surgical technique for thymic abnormalities (1). These techniques include transcervical approach, subxiphoid approach, unilateral (2) or bilateral thoracoscopic surgery, hand-assisted thoracoscopic surgery, robotic-assisted thoracoscopic surgery (3) or a combination of these approaches (4,5).
Over the past decade, uniportal VATS has increasingly attracted professional and public interest and been widely applied in the treatment of thoracic diseases. Suda et al. reported a uniportal technique using a subxiphoid approach for extended thymectomy in 2012 (6). With some modification to that technique, we report here our first six consecutive experience in performing subxiphoid uniportal thoracoscopic extended thymectomy. The maximum diameter of the thymic lesions in our group is 4 cm. We regard patients with poor lung function unable to withstand the selective one-lung ventilation, extensive pleural symphysis and thymic malignancy, or any sign of invasion as contraindications to using this approach for resection.
Although the limitations of this technique include decreased maneuverability of instruments, two-dimensional view of the surgical field and risk of breaching the tumor capsule, our recent experience demonstrates that subxiphoid uniportal approach is a satisfactory procedure for performing extended thymectomy in well selected patients. It provides simultaneous access to both pleural cavities, which greatly improves the view by split-lung ventilation. The procedure is safe and feasible, with good cosmesis, and the short-term results are promising.
Our clinical outcomes are limited to a small number of patients with relatively short follow-up time. To further evaluate the feasibility, safety, and efficacy of this technique, more experiences woud be required in well selected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ye B, Tantai JC, Ge XX, et al. Surgical techniques for early-stage thymoma: video-assisted thoracoscopic thymectomy versus transsternal thymectomy. J Thorac Cardiovasc Surg 2014;147:1599-603. [PubMed]
- Odaka M, Akiba T, Yabe M, et al. Unilateral thoracoscopic subtotal thymectomy for the treatment of stage I and II thymoma. Eur J Cardiothorac Surg 2010;37:824-6. [PubMed]
- Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011;141:673-7. [PubMed]
- Yu L, Ma S, Jing Y, et al. Combined unilateral-thoracoscopic and mediastinoscopic thymectomy. Ann Thorac Surg 2010;90:2068-70. [PubMed]
- Zielinski M, Czajkowski W, Gwozdz P, et al. Resection of thymomas with use of the new minimally-invasive technique of extended thymectomy performed through the subxiphoid-right video-thoracoscopic approach with double elevation of the sternum. Eur J Cardiothorac Surg 2013;44:e113-9; discussion e119.
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [PubMed]


