Incidental bronchial injury by soft coagulation
Introduction
Soft coagulation is a specific mode of VIO electrosurgical units (ERBE Elektromedizin, Tubingen, Germany), which provides dramatic hemostasis during various types of surgery. The most characteristic feature of this device, when compared with the ordinary electrosurgical units, is that it automatically regulates its output voltage below 200 V, which denatures the target protein between 70 and 80 °C. This low-temperature coagulation enables hemostasis of large blood vessels, without carbonizing or damaging the bleeding point and the surrounding tissue (1,2). In thoracic surgery, accidental damage to the surrounding organs, such as the pulmonary artery, leads to critical bleeding. Using this atraumatic device in thoracic surgery improves the safety of major pulmonary resection. We routinely use this device in our surgery as a countermeasure for unexpected intraoperative bleeding, using a ball electrode tip and setting the system at effect 5 and 60 W. Surgery has become safe and comfortable with the advent of this technology.
However, there are no reports describing the harmful effect of the above electrosurgical device in thoracic surgery. Here, we report intraoperative bronchial injuries caused by soft coagulation in three patients, and bronchopleural fistula (BPF) developed in one patient. This new device is a useful hemostatic tool, but some precautions are needed for its safe operation.
Case 1
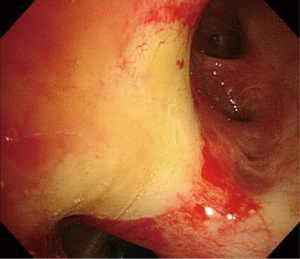
A 70-year-old man underwent lingular segmentectomy via thoracoscopic surgery (TS) for pulmonary aspergilloma. The bronchial artery (BA) was damaged while dissecting the interlobar lymph nodes during surgery. The electrode tip of the electrocautery device was kept in contact with the anterior bronchial wall at the second carina during hemostasis of the BA, using soft coagulation mode (Figure 1). The operation was accomplished without any other problems. Bronchoscopy on postoperative day 5 revealed ischemia in the anterior bronchial wall at the level of the second carina (Figure 2). Bronchial ischemia resolved on postoperative day 30, without BPF.

Case 2
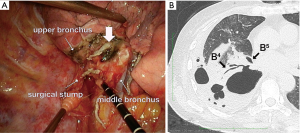
Right lower lobectomy via TS was performed for stage IA lung adenocarcinoma in a 66-year-old woman. Bleeding from the BA occurred during surgery when exposing the bronchus, adjacent to the lateral bronchial wall of the lateral segmental bronchus (B4), which was stanched using the soft coagulation mode (Figure 3A). Lobectomy was accomplished without any other complications. Thirteen days after the operation, the patient visited our emergency room for acute dyspnea. Chest computed tomography and bronchoscopy revealed a BPF of the middle lobar bronchus, at exactly the same site where the intraoperative bleeding was stanched, suggesting bronchial injury caused by electrocautery (Figure 3B). Thoracoplasty concomitant with plombage of the latissimus dorsi muscle was performed 1 month after open window thoracotomy. The patient was discharged from the hospital 50 days after the second admission.
Case 3
A 66-year-old man underwent right upper lobectomy via TS for stage IA lung adenocarcinoma. Bleeding occurred from the BA during right mediastinal lymph node dissection. Bleeding adjacent to the anterior wall of the right main bronchus was successfully stanched using the soft coagulation system. Intraoperative bronchoscopy after division of the upper bronchus revealed extensive ischemia of the anterior wall of the right main bronchus. To avoid postoperative BPF, we subsequently performed right sleeve upper lobectomy via posterolateral thoracotomy. Pathological study revealed a deep eschar in the cartilage portion of the right main bronchus. The postoperative course was good with no ischemic change in the anastomotic site and the surrounding bronchial mucosa. He was discharged 16 days after surgery.
Discussion
Soft coagulation systems provide major benefits to surgeons and patients. Previous studies have reported the efficacy of these devices in thoracic surgery, showing successful hemostasis of pulmonary and intercostal artery bleeding (1,2). However, there are only a few reports of the harmful effects of these devices. Kawai et al. reported a hypertensive crisis when using this device on adrenal tissue (4), but for thoracic surgery, there are no reports of the destructive effects caused.
Intraluminal damage of the bronchial wall caused by the soft coagulation system during endoscopic procedures was reported by Verkindre et al. in animal models. The bronchial damage appeared as whitish coagulation at 48 h, similar to the endoscopic findings of our case 1, which was observed microscopically as inflammation of the ulcerated mucosa, accompanied by edema of the submucosa and perichondral spaces. Evaluation at 6 weeks showed a persistent inflammatory lesion that extended deeply into the submucosa and perichondral spaces (as in our case 2). Some models died within the first 2 weeks from respiratory failure (5). The bronchial injuries that we observed in our study are considered equivalent to the previously described intrabronchial damage. Bronchial cautery induced by the soft coagulation system causes damage to the deep tissue layer, leading to a potential risk of bronchial wall perforation. Lung parenchyma and intercostal muscle, tissue adjacent to the pulmonary and intercostal arteries, have a high moisture content that prevents tissue damage from the coagulation heat burn. In contrast, structures with low moisture content, such as the cartilage portion of the bronchial wall, are easily damaged by coagulation heat, even under low temperature output. Therefore, careful evaluation of the bleeding point and the surrounding structure is necessary. The device described in the present cases is not suitable for bleeding from the BA near the bronchus. Surgeons must exercise caution when using this device for bleeding vessels adjacent to the airway cartilage.
Conclusions
We have described bronchial injury caused by a soft coagulation device in three patients. The soft coagulation mode of VIO electrosurgical units is an outstanding hemostatic device, but surgeons need special caution when using this device for bleeding adjacent to the trachea or bronchus.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Uchiyama A, Miyoshi K, Nakamura K. VIO soft-coagulation system for major pulmonary resections: results in 68 patients with primary lung cancer. Gen Thorac Cardiovasc Surg 2011;59:175-8. [PubMed]
- Sakuragi T, Ohma H, Ohteki H. Efficacy of SOFT COAG for intraoperative bleeding in thoracic surgery. Interact Cardiovasc Thorac Surg 2009;9:767-8. [PubMed]
- Shibano T, Endo S, Otani S, et al. Hemostasis using the soft coagulation mode of the electrosurgical unit. Asvide 2015;2:084. Available online: http://www.asvide.com/articles/677
- Kawai T, Suzuki M, Otsuka M, et al. Hypertensive crisis during hemostasis of adrenal bleeding using a soft-coagulation device. Int J Urol 2015;22:799-800. [PubMed]
- Verkindre C, Brichet A, Maurage CA, et al. Morphological changes induced by extensive endobronchial electrocautery. Eur Respir J 1999;14:796-9. [PubMed]


