Minimally invasive esophageal resection and intrathoracic anastomosis for lower thoracic esophageal cancer with single position
Introduction
Esophagectomy is a complex surgery aiming to remove an esophageal tumour and to create a new gastric tube, and the adoption of minimally invasive esophagectomy with chest anastomosis has increased worldwide due to the advantages of endoscopic techniques (1,2). We describe our use of laparoscopy and thoracoscopy to treat the lower thoracic esophageal cancer with single-position, and it shows the advantages on not only the preparation of the gastric tube and the mobilisation of the esophagus, but also the intrathoracic anastomosis of the esophagogastrostomy can be performed in a comfortable way.
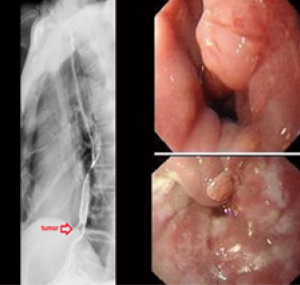
A 68-year-old male, with no notable medical history, was admitted to our hospital due to dysphagia for 1 year. Before the operation, a chest computed tomography (CT) scan reconstruction identified the abnormal mass on lower thoracic esophageal. A biopsy was conducted by gastroscopy (Figure 1), and the pathology identified the esophageal carcinoma. Then the patient underwent tumor radical resection using a single-position, minimally invasive surgical technique with laparoscopy and thoracoscopy (Figure 2), with the final histopathology showing the esophageal differentiated adenocarcinoma, negative margin. Postoperative courses are uneventful, clinical and radiologic follow-up 3 months after surgery showed excellent morphological and functional outcome.
Operative techniques
The patient was maintained in the supine position and the right chest was elevated by 30°. In the operating theatre, three laparoscopic ports were placed in the abdominal wall. We detected the specific position of the tumor, and confirmed the target lesion based on the preoperative chest CT. The mobilization of the stomach and lower esophagus and the abdominal lymphadenectomy were performed laparoscopically, without a pyloroplasty.
Then the thoracic procedure was performed through a single port with the use of thoracoscopy. A 5-cm incision was created at the clavicular line in the fifth intercostal space. Tilt the surgical bed to the left to get better chest exposure. The thoracoscopic esophageal mobilisation and mediastinal lymphadenectomy were performed with left lung ventilation. The anticipated location of the anastomosis on the esophagus was 5 cm higher than the superior edge of the tumor. A full-layer purse string of the esophagus was hand-sewn with prolene line. After the anvil head was inserted, the purse line was tightened and then the esophagus was transected, followed by a mini-laparotomy from where we pull out the stomach and the lower segment of the esophagus for the preparation of the gastric tube in vitro. We removed part of the lesser curvature of the stomach and the cardia, as well as the lymphoid adipose tissue of the lesser curvature.
Finally, the reconstruction was performed. A 3-cm incision of the anterior aspect of the stomach was made 10 cm distal to the esophagogastric junction to put the stapler in. The stomach was delivered to the chest in the right direction through the mini-laparotomy of abdominal wall, esophageal hiatus into the chest in turn, without torsion or tension, and then the gastro-esophageal anastomosis was created in the chest. Turn back the surgical bed to resume supine position. Removed the staple form the mini-laparotomy of abdominal wall and the staple line of the conduit and the anastomotic stoma were reinforced with interrupted 1# sutures at 1 cm intervals. Then the stomach tube and the nasogastric tube were routinely placed. Closed all the incisions.
Comments
Open approaches to esophagectomy include transhiatal, Ivor-Lewis, left thoracoabdominal, and McKeown, each with inherent advantages and disadvantages (4). Currently, minimally invasive approaches to esophagectomy have been adopted in an effort to reduce some of the complications associated with the open procedures (5). But it may have the disadvantage of increased operative time associated with repositioning.
In this case, a minimally invasive esophagectomy was successfully performed in a single position (supine), and it has the advantages of endoscopic techniques as less discomfort, shorter length of stay and a faster recovery to baseline status. In addition, this approach provides excellent exposure of the esophagus and intrathoracic visualization, allowing for distal mediastinal and celiac lymphadenectomy in one position. In particular, using the mini-laparotomy incision, the gastric tube was created in vitro, and then delivered to the chest through esophageal hiatus, followed the intrathoracic gastro-esophageal anastomosis without putting the anastomat through the thoracic incision, thus not only reducing the potential contamination within the chest, but making the procedure performed in a comfortable way and also save a lot of time compared with laparoscopic operation. Another improvement of using the mini-laparotomy incision is that it avoided the anastomat entering into the chest operation hole, thus reducing the potential injury of the intercostal nerve. Moreover, the nasogastric tube was routinely placed as open approach, so it omitted the procedure of jejunostomy. We introduce a previous report to help explain the operation (6). However, compared with the surgical method taken for the case in the article above, we make further improvement for the case in this report. Only one observation hole below the umbilicus and two operating holes on the right abdomen are needed for the abdominal operation, while single hole on the chest is changed to be taken on the fifth rib that is more minimal invasive than the previous one.
Before this case, all cases we selected for the treatment group of this surgical procedure are esophageal squamous carcinoma. It is mainly because squamous carcinoma is the most frequently occurring esophagus cancer in China, while there are a small number of cases caused by adenocarcinoma. Until now our team has no experience to perform the operation on cases of esophageal adenocarcinoma except this case. The tumor of the case in the treatment group was located above dentate line and below the edge of inferior pulmonary veins. In our experience, the distance from tumor to esophageal hiatus is a relatively minor factor. Since the distal margin from the lower border of tumor would be formed tubular stomach at the same time as both cardia and lesser curvature of stomach are removed through abdominal incision, the location does not affect the operation within thoracic cavity. But the amputated proximal margin should be done in thoracic cavity, which demands the distance to be ensured. Therefore we believe the condition that the location is below the edge of inferior pulmonary veins is an important sign of judgment.
Thus, we consider that the procedure described could be very a viable alternative for patients with lower thoracic esophageal cancer which seems to be more minimally invasive.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- Nguyen NT, Follette DM, Lemoine PH, et al. Minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2001;72:593-6. [PubMed]
- Burdall OC, Boddy AP, Fullick J, et al. A comparative study of survival after minimally invasive and open oesophagectomy. Surg Endosc 2015;29:431-7. [PubMed]
- Zhao L, Ge J, Li W, et al. Minimally invasive oesophageal resection and intrathoracic anastomosis for lower thoracic oesophageal cancer with single position. Asvide 2015;2:085. Available online: http://www.asvide.com/articles/678
- Parascandola SA, Marshall MB. Minimally invasive thoracoabdominal esophagectomy in a morbidly obese patient. Ann Thorac Surg 2014;98:e19-21. [PubMed]
- Wu W, Zhu Q, Chen L, et al. Technical and early outcomes of Ivor Lewis minimally invasive oesophagectomy for gastric tube construction in the thoracic cavity. Interact Cardiovasc Thorac Surg 2014;18:86-91. [PubMed]
- Zhang G, Liang C, Shen G, et al. Single-position, minimally invasive Ivor Lewis oesophagectomy for lower thoracic oesophageal cancer. Eur J Cardiothorac Surg 2014;46:1032-4. [PubMed]


