A case of recurrent pneumothorax related to oral methylphenidate
Introduction
Primary spontaneous pneumothorax (PSP) is considered when there is no identifiable pulmonary parenchymal abnormality, except for emphysema-like changes (ELCs; i.e., blebs and bullae) in a patient presenting with spontaneous pneumothorax. PSP has an annual incidence of approximately 18 to 28 per 100,000 male populations (1). Male gender (particularly young males), tall and thin stature, cigarette smoking, and family history are well-known risk factors of PSP (2,3). However, other risk factors may be overlooked. Herein, we report on a 19-year-old man who presented with multiple episodes of spontaneous pneumothorax while taking oral methylphenidate.
In 2013, a 19-year-old man was referred to our hospital for further evaluation of multiple episodes of spontaneous pneumothorax. The first episode occurred in 2011 on the patient’s left side and then repeatedly on both sides even though video-assisted thoracoscopic surgery (VATS), blebectomies and pleurodesis by mechanical pleural abrasion were performed several times. Only simple lung blebs were found during pathological examination of resected lung specimens.
In 2010, the patient was diagnosed with attention deficit hyperactivity disorder and was treated with oral methylphenidate 10 mg twice daily thereafter. He had never smoked cigarettes and denied a history of drug abuse. There was no family history of PSP, including his elder brother.
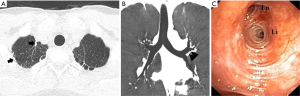
Physical examination was unremarkable. The patient was 178 cm tall and weighed 64 kg but did not have a marfanoid appearance. Pulmonary function test was normal. Computed tomography (CT) of the chest revealed multiple small subpleural blebs/bullae in the left apical lung (Figure 1A). In addition, there were multiple tiny out-pouching lesions arising from the lobar and segmental bronchi of all pulmonary lobes (Figure 1B). There was no evidence of basilar panlobular emphysema. Bronchoscopic examination confirmed the presence of diffuse bronchial diverticulosis involving multiple lobar and segmental bronchi, bilaterally (Figure 1C).
Following an extensive literature review, we speculated that oral methylphenidate could be the potential cause of recurrent spontaneous pneumothorax in this patient. Therefore, the patient was counseled to stop taking this medication (in June 2013). After methylphenidate discontinuation, there was no new or recurrent episode of pneumothorax. Nevertheless, follow-up chest CT and bronchoscopy obtained 1 year later showed persistence of bilateral lung blebs and bronchial diverticulosis.
Discussion
Although the present case had evidence of ELCs—the hallmark and predisposing factor of PSP—found on chest CT and resected lung specimens, he continued to have recurrent pneumothorax after undergoing repeated surgical pleurodesis and blebectomies. Therefore, it would be seem that another etiology must account for the development of recurrent spontaneous pneumothorax in this patient.
Methylphenidate is an oral medication for treating neuropsychiatric diseases. Some previous reports have implicated methylphenidate as the cause of basilar panlobular emphysema among intravenous abusers (4-6). The pathogenesis and development of panlobular emphysema in these cases remains unclear: whether it is triggered by the drug per se, or as a consequence of repeated microemboli caused by the components in crushed tablets. Greater blood flow to the lung bases may well explain the basal location of emphysema in these patients (5). Ward et al. demonstrated a significantly higher prevalence of basilar panlobular emphysema in drug abusers using intravenous methylphenidate compared with those abusing other oral drugs (7). Moreover, there was a reduction of elastic fibers and decreased interstitial fibrosis in the lung specimens of intravenous methylphenidate abusers compared with other intravenous abusers (5). Methylphenidate was also found to be associated with reversible growth inhibition and bone quality impairment (8). These observations might support the hypothesis that methylphenidate itself could be the primary causal agent of pneumothorax, both in those patients and in the present case. Despite the differences in routes of drug administration and CT findings, we speculate that long-term treatment with oral methylphenidate may have aggravated the rupture of the preexisting ELCs in our patient, leading to pneumothorax. This hypothesis has recently been supported in animal model. Rapello et al. demonstrated destruction of the alveolar septa in the lung parenchyma of Wistar rats after gavage feeding with a therapeutic dose of methylphenidate for 90 days (9).
Bronchial diverticulum is characterized by mucosal depression and prolapse of the bronchial mucosa through the dehiscent muscular bundles in the bronchus. It could be detected in the elderly, in cigarette smokers, and in patients with chronic obstructive pulmonary disease or with a connective tissue disorder such as Mounier-Kuhn syndrome (10). In the absence of the aforementioned risk factors and any other probable causes, bronchial diverticulosis in our patient might also be attributed to methylphenidate, which could be explained by the same pathogenesis of ruptured ELCs as proposed above. Nevertheless, additional case reports and further investigations are required before the conclusion can be made.
In summary, we report a first case of recurrent spontaneous pneumothorax that might be related to long-term administration of oral methylphenidate. Although the relationship and pathogenesis remain unclear, the clinician should be aware of the possibility of oral methylphenidate-induced pneumothorax in any patient presenting with spontaneous pneumothorax while taking this drug. Hence, methylphenidate should be prescribed with caution, especially in a young, thin, and tall patient.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tschopp JM, Rami-Porta R, Noppen M, et al. Management of spontaneous pneumothorax: state of the art. Eur Respir J 2006;28:637-50. [PubMed]
- Bintcliffe O, Maskell N. Spontaneous pneumothorax. BMJ 2014;348:g2928. [PubMed]
- Currie GP, Alluri R, Christie GL, et al. Pneumothorax: an update. Postgrad Med J 2007;83:461-5. [PubMed]
- Sherman CB, Hudson LD, Pierson DJ. Severe precocious emphysema in intravenous methylphenidate (Ritalin) abusers. Chest 1987;92:1085-7. [PubMed]
- Schmidt RA, Glenny RW, Godwin JD, et al. Panlobular emphysema in young intravenous Ritalin abusers. Am Rev Respir Dis 1991;143:649-56. [PubMed]
- Stern EJ, Frank MS, Schmutz JF, et al. Panlobular pulmonary emphysema caused by i.v. injection of methylphenidate (Ritalin): findings on chest radiographs and CT scans. AJR Am J Roentgenol 1994;162:555-60. [PubMed]
- Ward S, Heyneman LE, Reittner P, et al. Talcosis associated with IV abuse of oral medications: CT findings. AJR Am J Roentgenol 2000;174:789-93. [PubMed]
- Komatsu DE, Thanos PK, Mary MN, et al. Chronic exposure to methylphenidate impairs appendicular bone quality in young rats. Bone 2012;50:1214-22. [PubMed]
- Rapello GV, Antoniolli A, Pereira DM, et al. Pulmonary emphysema induced by methylphenidate: experimental study. Sao Paulo Med J 2015;133:131-4. [PubMed]
- Miyara T, Oshiro Y, Yamashiro T, et al. Bronchial diverticula detected by multidetector-row computed tomography: incidence and clinical features. J Thorac Imaging 2011;26:204-8. [PubMed]


