Primary squamous cell carcinoma in the chest wall mimicking abscess
Introduction
Diagnosis of chest wall tumors is challenging because their imaging features can be nonspecific. Their accurate diagnosis provides opportunities for complete resection and collaboration reconstruction. We report a case of primary squamous cell carcinoma (SCC) arising from chest wall.
Case report
A 53-year-old female had an asymptomatic small uptake on her right chest wall on PET-computed tomography (CT) (Figure 1A) by a medical-checkup. She had a 5-year history of type 2 diabetes that had been treated with metformin 500 mg. Ultrasonography revealed a 0.8-cm indistinct hypoechoic mass in the pectoralis muscle abutting the manubrium. Ultrasonography-guided fine-needle aspiration was performed. The pathology revealed a reactive lymphoid hyperplasia. Eight months later, the mass did not show any change and there was no mammographic abnormality. She was not followed for two years. However, at a later date, she was suddenly admitted due to pain. Ultrasonography demonstrated a large cystic mass arising from her chest wall (Figure 1B). We initially diagnosed it as an abscess but pathology result was carcinoma by fine-needle aspiration.
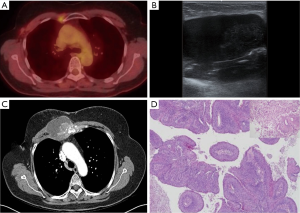
To evaluate the tumor, CT scans was performed, which revealed a 7.5 cm × 5.4 cm × 8.5 cm, infiltrative heterogeneous enhancing mass with bony destructions of the sternum and the 1st to 3rd ribs (Figure 1C). Histopathology revealed a moderately differentiated SCC through an excisional biopsy (Figure 1D). An immunohistochemical evaluation was negative for ER, PR, and HER 2 and positive for EGFR and Ki-67 (60%).
Neither inspection of the skin nor whole-body CT scan could detect any primary lesions. She received adjuvant chemotherapy with cisplatin 93 mg/m2 plus 5-fluorouracil 1,860 mg/m2 which is commonly used in combination for SCC of other organs such as the head and neck, the breasts, and the anus. Afterwards, she underwent a complete wide excision including a sternotomy and had a reconstruction with bone cement and prolene mesh performed by a plastic surgeon. The surgical specimen was proved pathologically as a SCC of the chest wall with invasion of the ribs and sternum. She also underwent external beam radiation therapy consisting of five consecutive daily fractions per week with a fraction size of 1.8-2.0 Gy. Total dose was 64.8 Gy. She has been followed up for 1 year with no clinical or radiological evidence of recurrence.
Discussion
Differential diagnosis between metastatic carcinoma and primary soft-tissue tumor is critical because treatment and prognosis are markedly different. Malignant chest wall tumors are a heterogeneous group of tumors including invasion from an adjacent tumor, primary tumor, and metastatic tumors. Invasion from adjacent tumor that occur in the lung or breast are relatively more common than others (1).
Primary chest wall tumor can be classified into bone or soft tissue tumor. A bulky mass invading adjacent structures without mineralization is suspected to be malignant soft tissue tumor. In adults, malignant fibrous histiocytoma (MFH) is the most common. MFH arises in the deep fascia or skeletal muscle in elderly people. It is usually a painless mass regardless of how large it is. CT finding can reveal a heterogeneous enhancing or calcified mass.
In consideration of pain, neurofibrosarcomas are suspected but they are usually associated with neurofibromatosis type I. They grow along the major or medium-sized nerves such as the sciatic nerve, brachial or sacral plexuses.
Squamous cells may arise from luminal epithelial cells, myoepithelial cells, or ductal metaplasia (2). SCC is characterized by numerous malignant squamous cells with keratinizing eosinophilic glassy cytoplasm, intercellular bridges, keratin debris and background necrosis. To confirm the diagnosis, a surgical biopsy is mandatory.
Abscess present as a painful, cystic lesion with erythema. It is generally accepted that patients with diabetes mellitus are more susceptible to an unusual site infection. Our case was a chest wall lesion mimicking an abscess in a patient who had a history of diabetes. Specific findings and most appropriate chemotherapeutic regimen for an SCC are unclear because of their rarity. Limited literature has reported that SCC occurs in flaps which are used for reconstruction and chest resections (3,4). A case of the published literature reported that a combination of cisplatin and 5-fluorouricil was effective for SCC (5,6). Our patient also responded to combination treatment.
Imaging diagnoses may be difficult because of non-specific findings of chest wall tumors. However, if tumors are presented as rapidly growing cystic masses without any adenopathy or calcifications in elderly patients, SCC should be considered in differentials diagnoses and adequate treatments must be carried out.
Acknowledgements
This study was supported by the Inha University research grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Thomas-de-Montpréville V, Chapelier A, Fadel E, et al. Chest wall resection for invasive lung carcinoma, soft tissue sarcoma, and other types of malignancy. Pathologic aspects in a series of 107 patients. Ann Diagn Pathol 2004;8:198-206. [PubMed]
- Dejager D, Redlich PN, Dayer AM, et al. Primary squamous cell carcinoma of the breast: sensitivity to cisplatinum-based chemotherapy. J Surg Oncol 1995;59:199-203. [PubMed]
- Mohan AM, Balaguhan B, Krishna V, et al. Squamous cell carcinoma of the pectoralis major myocutaneous flap donor site. J Oral Maxillofac Surg 2014;72:1425-31. [PubMed]
- Kotani K, Makihara S, Tada R. Squamous cell carcinoma of the chest wall in a patient with chronic empyema. Kyobu Geka 2011;64:549-51. [PubMed]
- Mitra B, Pal M, Debnath S, et al. Primary squamous cell carcinoma of breast with ipsilateral axillary lymph node metastasis: An unusual case. Int J Surg Case Rep 2011;2:194-7. [PubMed]
- Collado Martín R, García Palomo A, de la Cruz Merino L, et al. Clinical guideline SEOM: cancer of unknown primary site. Clin Transl Oncol 2014;16:1091-7. [PubMed]


