Clinical experience with titanium mesh in reconstruction of massive chest wall defects following oncological resection
Introduction
Malignant tumors of the chest wall are uncommon, which can be generally classified as primary, locally invading, and metastatic lesions. Wide surgical resection with margin negativity by removing both of the chest wall tumor and adjacent tissues is considered to prolong the survival and decrease the recurrence significantly, which is prone to result in large defects, though (1). Thus, reconstruction of the wide defect is needed, the goals of which are adequate stability to prevent paradoxical movement and protect intrathoracic organs as well as acceptable cosmetic appearance.
Advancements in surgical reconstruction techniques, including the employment of pedicled musculocutaneous flaps and/or various prosthetic materials make it possible to perform radical resections with eliminating the lesions, and good long-term survival (2-4). Despite the unremitting efforts, there was no consensus on the determination which approach to choose, mainly depending on the surgeon’s preference. The use of titanium-based devices, such as titanium clips, bars, plates and screws for chest wall reconstruction or ribs fractures fixation have been largely demonstrated, which could provide well-established chest stability and flexibility (3,5). Clinically, titanium mesh was widely used in the repair of skull defects (6). Currently, only a few case reports with respect on its applications in chest wall reconstruction were presented (7,8). We have reported a satisfactory application of titanium mesh in an aged woman with complex and major chest wall defects after removal of a lower-sternal mass in 2009 (9). Herein, the experience with titanium mesh to restore skeletal defects following radical chest wall tumor resections in our single institution was reviewed. Patients’ and tumors’ characteristics, the extent of the resection, resulting defects and postoperative complications as well as long-term follow-up were discussed.
Materials and methods
All patients had massive musculoskeletal defects reconstructed with titanium mesh in Shanghai Chest Hospital, between January 2009 and August 2014. All were presented with chest wall malignancies performed in a single-stage procedure.
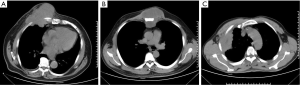
Titanium mesh was used when the defect in the chest wall was larger than 6 cm or ≥3 ribs. Before surgery, emission computed tomography (ECT), chest computed tomography (CT) scan (Figure 1) and pulmonary function tests were routinely used in all patients. The metastatic work-up was undertaken to eliminate an extrathoracic metastatic lesion. A total of 27 patients were identified, forming the basis of this review. Patients’ and tumors’ records were collected.
The surgical procedure
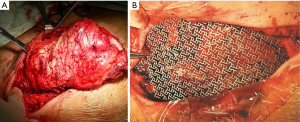
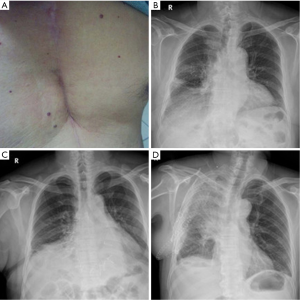
Double-lumen endobronchial tube was inserted following general anesthesia. The chest wall tumors and involved chest wall (including ribs and adjacent soft tissue) with at least 4 cm margin were totally removed (Figure 2). Subcutaneous tissue and skin were not removed. For relatively small resections, direct closure is performed, given that skin and subcutaneous tissue can be preserved with a good blood flow so that a titanium mesh can be safely covered. For lager defections, regional pedicled muscular or musculocutaneous flaps were used as choice for soft tissue coverage of the titanium meshes. Microscopic evaluation of the margins by frozen section was not routinely made due to wide resection. Titanium mesh prosthesis [Timesh (Flexmesh), Medtronic neurologic technologies] with tailored size was placed in the defect. Each side of the prosthesis overlapped the edge of the defect by 1-2 cm and was fixed with steel wires around the end of the resected ribs and/or sternum, as shown in Figure 1. The chest cavity was drained with a 28F chest tube. Subcutaneous drainage was not used in the mesh site. Pressure dressing was routinely used while not respiratory support postoperatively.
Follow-up
The first visit was at the fourth week postoperatively and then patients were seen every 3 months in the first year and subsequently every 6 months. Chest stability, skin appearance, relief of symptoms and the status of tumors were evaluated. Visual analogue scale (VAS) was used for pain measurement at the first visit. 0 indicates no pain, with 10 representing the most severe and unbearable pain. Point between 0 and 2 is classified as ‘excellent’, ‘3-5’ as ‘good’, ‘6-8’ as ‘tolerable’, and ‘8-10’ as ‘poor’. Local recurrence was defined as appearance of the same tumor in the previously surgical site, which was confirmed by needle aspiration biopsy. All survival and recurrence data were calculated from the date of surgical resection. The Kaplan-Meier method was used for overall survival (OS) and disease-free survival (DFS) analysis.
Results
Clinical presentation
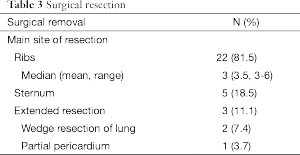
Patients’ characteristics were described in Table 1. Overall, 27 patients (16 males vs. 11 females, mean age 48 years, range, 14-76) were identified. Most patients were symptomatic with pain (77.8%) and examination finding a palpable mass (14.8%). The average tumor size and mesh dimensions were 72.4 (range, 36-140) cm3 and 140.9 (range, 80-225) cm2, respectively. The mean blood loss and operation time were 201.9 (range, 100-600) mL and 126.7 (range, 70-240) minutes, respectively. No perioperative mortality was recorded and mean postoperative stay was 7.1 (median 6, range, 4-14) days. Postoperative course was uneventful in 24 (85.2%) patients, and 4 (14.8%) patients developed postoperative complications. Two cases had pneumonia/atelectasis, and one of them required temporarily assisted ventilation, breathing normally and independently after 36 hours. Two patients had seroma in the surgical sites, due to aneuros compression bandage. Abnormal respiratory movement caused by chest wall instability was not observed.
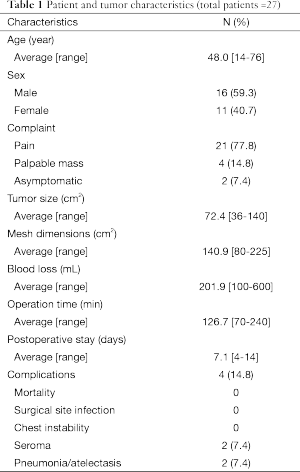
Full table
Histopathological distributions of chest wall neoplasms were presented in Table 2. Primary chest wall tumors were the most frequent (n=21, 77.8%), including chondrosarcoma (n=7), fibrosarcoma (n=4), desmoid tumor (n=3), liposarcoma (n=3), Ewing sarcoma (n=1), plasma cell tumors (n=1), synovial sarcoma (n=1) and osteosarcoma (n=1). Of those, four cases (two with fibrosarcoma and two with desmoid tumor) were referred from outside institutions presented with recurrence due to intralesional resections. Squamous cell lung cancer (SCLC) (n=4), locally recurrent breast carcinoma (n=1), anterior mediastinum-derived Hodgkin lymphoma (n=1) constituting the secondary chest wall malignancies (n=6, 22.2%) of our series.
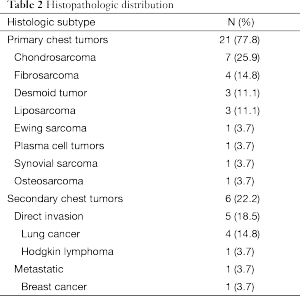
Full table
The resulting chest wall resections were listed in Table 3. All patients underwent wide surgical removal. Resection of ribs and adjacent soft tissue were performed in 22 (81.5%) patients, including the anterior (n=13), and lateral (n=9) chest wall resection. The number of ribs resection was range from 3 to 6 (median 3, mean 3.5). Combined partial resections of sternum and adjacent costal cartilages were performed in five (18.5%) patients. In addition, the extended wedge resection of the lung and partial resection of the pericardium were performed in two cases (one with sternal chondrosarcoma and one with Ewing sarcoma) and one case (chondrosarcoma), respectively.
Full table
Follow-up
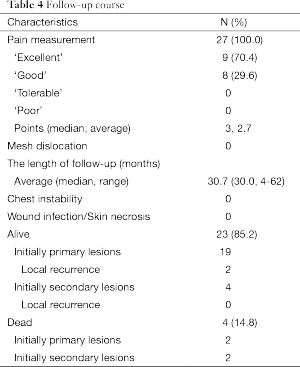
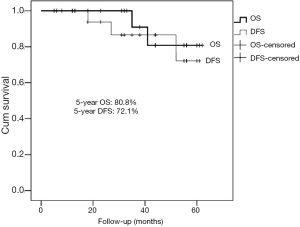
Table 4 summarized the postoperative follow-up course of all patients. The mean follow-up was 30.7 months (median 30.0 months, range, 4-62 months). All patients were seen every 3 months in the first year and then every 6 months, showing satisfactory cosmetic and functional outcomes (Figure 3A). During the course, none of the patients had experienced paradoxical respiratory motion or wound infection or skin necrosis. Furthermore, there was no mesh dislocation (Figure 3B-D). All patients performed VAS for pain measurement showed ‘excellent’ or ‘good’ outcomes points (median 3, average, 2.7). At the last follow-up, 23 patients were alive (19 with initially primary lesions and 4 with initially secondary lesions). Of those, two cases with local recurrence (one with fibrosarcoma and one with desmoid tumor) were observed at 52 and 27 months, respectively. Four died (two with initially primary disease including one with osteosarcoma, and one with sternal plasma cell tumors; two with secondary disease including one with Hodgkin lymphoma and one with squamous cell lung carcinoma). One died of both local recurrence and distant metastasis. Three cases of death were unknown. The 5-year DFS and OS of primary chest tumors was 72.1% and 80.8%, respectively (Figure 4).
Full table
Discussion
In large defect reconstruction following radical resection of malignant chest wall tumors, properly structural chest wall reconstruction with stability, integrity, and aesthetics should be ensured. It is technically challenging because of the residual large defect after radical resection and its inherent rarity of the tumors. The refinements in the reconstruction techniques have allowed wide chest wall resections to be performed with acceptable morbidity and mortality.
The chest wall malignancies include primary or secondary chest wall neoplasms, with a dominance of sarcoma and relapse breast cancer, respectively (10). In this study, primary chest wall tumors were the most common (77.8%), which were mainly consisted of chondrosarcoma and fibrosarcoma. The most frequent in secondary tumors was the SCLC. The difference could be explained by the selection bias and the situation that the most taken in our department were patients with lung cancers.
The size of the chest wall defect was directly related to postoperative complications due to impaired respiratory function and instability of chest. Stabilization of chest wall with a rigid prosthesis following extensive resections is considered to be effective to prevent the occurrence of flail chest and to improve postoperative pulmonary function. The selection of the prosthesis whether or not is mainly influenced by the site and the size of the defect. In our department, patients with the resections of ≥3 ribs or 6 cm were considered to be the candidates for prosthesis reconstruction, generally. For defects in sternal and parasternal sites, especially skeletal tissue of the praecordia, rigid prosthesis is important to maintain the structural integrity, to prevent chest wall to collapse and to protect the intrathoracic organs. For defects located under the dorsal scapular bone, a prosthesis is dispensable given the rigid protection of scapula.
A desirable prosthetic material for chest wall reconstruction was considered to have the following characteristics: enough strength to prevent paradoxical chest motion, nice biocompatibility to allow in-growth of tissue, good flexibility to be fashioned into the appropriate shape and excellent radiolucency to allow radiographic follow-up (11). Prosthesis like Marlex mesh, Vicryl and ePTFE materials in the reconstruction of medium defects have been largely utilized, generally based on the surgeon’s experience and preference (12,13). Polypropylene mesh (Marlex) is the most popularly used. It is relatively cheap and has a good affinity for tissue growth, but its lack of enough rigidity in patients with extensive defects may result in paradoxical motion of the chest wall.
In our series, titanium mesh, which can provide enough rigidity and has good flexibility and biocompatibility, was selected in 27 patients with wide chest wall defections following radical oncological resection, given the possibly resulting instability with use of Vicryl prosthesis. The surgical outcomes were satisfactory with acceptable postoperative complications, comparable or even superior to several other reports (14,15). In the absence of subcutaneous drain, no wound infection or necrosis occurred and most of them recovered smoothly in our series. Two cases with seroma were reported in our series owing to slack compression bandage, which were solved with satisfaction by careful dressing and compression bandaging. Pneumonia/atelectasis occurred in two cases with lung cancers following combined lobectomy and chest wall resection, which might be associated with the excessive trauma. Cosmetic and functional outcomes were satisfactory in all patients, and there was no obviously unpleasant pain and discomfort during the follow-up.
Beneficial resection margin has been largely discussed since the extent of resection is closely associated with a radical resection, which was crucial to prolong survival and reduce recurrence postoperatively (11). Inclusion of one additional healthy rib superiorly and inferiorly as well as intercostals muscles in primary chest sarcoma was suggested by King et al. (16), following which Warzelhan et al. (10) achieved a 58% 5-year OS in chest wall sarcomas. Simply negativity in frozen sections without specific distance was considered safe enough, according to Novoa et al. (13). Although wide surgical resection was thought as a significant prognostic factor, the type of surgical resection (wide or marginal) did not significantly influence the OS, according to Gross and colleagues (17). In reports by Billè (15), resections of chest wall tumors were performed with a margin of at least 5 cm, while the resulting recurrence or survival was not shown. Following 3-cm margin principle, Gonfiotti et al. (18) achieved tumor free margins of all cases with a 5-year OS of 61% and two cases with recurrence during a mean follow-up of 60.5 months. More recently, an at least 3-cm free margin proximally and distally to the chondrosarcoma was demonstrated with desirable results: 5-year OS and DFS rates were 67.1% and 70%, respectively (11). The prognosis of chest wall tumors appeared to become better during the last decades due to a wider resection (19). Currently, many institutions shift towards more extended procedures for chest wall tumours, thanks to the available improvements of reconstructive techniques, which allow more excessive resection. Thus, it was accompanied by a dramatic decrease in the number of incomplete or intralesional resections. As a result, local control improved significantly and ultimately it also affected the outcome. There was a more frequent use of titanium mesh in our department in the past several years, permitting wide resections with at least 4-cm healthy tissues along with the lesions and ensuring enough strength simultaneously. In our series, the 5-year disease-free and overall survivals of primary chest tumors were 72.1% and 80.8%, respectively. Surgical resection with tumor-free margins should be attempted whenever feasible, while the role of chemotherapy and/or radiation remained unclear (19). Few of the primary chest wall tumors appeared to be radiosensitive. Given all the reachable wide resection, there were no routinely adjuvant therapies used in our series, except for Ewing sarcoma, osteosarcoma, aggressive SCLC and breast cancer as well as Hodgkin lymphoma. However, patients who were at high risk of local recurrence or compromised margins might benefit from adjuvant treatment. The appropriateness of (neo) adjuvant therapy is worth a further multidisciplinary discussion (20).
Taken together, the employment of titanium mesh for reconstruction of chest wall has the following advantages: (I) it has characteristics of good plasticity and tenacity as well as light-weight, compatible with the radian of chest wall well, and more importantly, it provided enough stability and allows wide resections; (II) its biocompatibility is excellent and unpleasant symptoms are not complained; (III) the magnetic compatibility of the prosthesis after implantation is good, without affecting the CT, MRI (magnetic resonance imaging), or DSA (digital subtraction angiography) inspections, etc.; (IV) there is no routine need to place subcutaneous drain, and subcutaneous effusion can flow into the chest transthoracic tube; (V) it is easier to shape, and the operation is faster and easier, only requiring several sutures with steel wires placed in an interrupted fashion around the ribs.
Several limitations of this study deserve mention. The rarity and heterogeneity of these tumors, and the absence of a comparative material, have limited analyses. The most obvious flaw of this retrospective study is the inherent selection bias, with surgical reconstruction being simply performed for chest wall defects following oncological resection.
Conclusions
We described a technique for the reconstruction of wide chest wall defects using titanium mesh. Its characteristics were related with light-weight, nice flexibility but excellent strength (superior strength-to-weight ratio), good biocompatibility as well as magnetic compatibility, and it was preferred to be used in wider chest wall defects, all of which signified safe and prospect in utilization with good patient outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wouters MW, van Geel AN, Nieuwenhuis L, et al. Outcome after surgical resections of recurrent chest wall sarcomas. J Clin Oncol 2008;26:5113-8. [PubMed]
- Puviani L, Fazio N, Boriani L, et al. Reconstruction with fascia lata after extensive chest wall resection: results. Eur J Cardiothorac Surg 2013;44:125-9. [PubMed]
- Turna A, Kavakli K, Sapmaz E, et al. Reconstruction with a patient-specific titanium implant after a wide anterior chest wall resection. Interact Cardiovasc Thorac Surg 2014;18:234-6. [PubMed]
- George RS, Kostopanagiotou K, Papagiannopoulos K. The expanded role of extracellular matrix patch in malignant and non-malignant chest wall reconstruction in thoracic surgery. Interact Cardiovasc Thorac Surg 2014;18:335-9. [PubMed]
- Matsumoto K, Sano I, Nakamura A, et al. Anterior chest wall reconstruction with titanium plate sandwiched between two polypropylene sheets. Gen Thorac Cardiovasc Surg 2012;60:590-2. [PubMed]
- Manjila S, Weidenbecher M, Semaan MT, et al. Prevention of postoperative cerebrospinal fluid leaks with multilayered reconstruction using titanium mesh-hydroxyapatite cement cranioplasty after translabyrinthine resection of acoustic neuroma. J Neurosurg 2013;119:113-20. [PubMed]
- Koto K, Sakabe T, Horie N, et al. Chondrosarcoma from the sternum: reconstruction with titanium mesh and a transverse rectus abdominis myocutaneous flap after subtotal sternal excision. Med Sci Monit 2012;18:CS77-81. [PubMed]
- Ersöz E, Evman S, Alpay L, et al. Chondrosarcoma of the anterior chest wall: surgical resection and reconstruction with titanium mesh. J Thorac Dis 2014;6:E230-3. [PubMed]
- Liu ZC, Zhao H. Titanium internal fixation system used for sternum reconstruction after resection of chondrosarcoma. Chin Med J (Engl) 2010;123:2621-2. [PubMed]
- Warzelhan J, Stoelben E, Imdahl A, et al. Results in surgery for primary and metastatic chest wall tumors. Eur J Cardiothorac Surg 2001;19:584-8. [PubMed]
- le Roux BT, Shama DM. Resection of tumors of the chest wall. Curr Probl Surg 1983;20:345-86. [PubMed]
- Marulli G, Duranti L, Cardillo G, et al. Primary chest wall chondrosarcomas: results of surgical resection and analysis of prognostic factors. Eur J Cardiothorac Surg 2014;45:e194-201. [PubMed]
- Novoa N, Benito P, Jiménez MF, et al. Reconstruction of chest wall defects after resection of large neoplasms: ten-year experience. Interact Cardiovasc Thorac Surg 2005;4:250-5. [PubMed]
- Khalil el-SA, El-Zohairy MA, Bukhari M. Reconstruction of large full thickness chest wall defects following resection of malignant tumors. J Egypt Natl Canc Inst 2010;22:19-27. [PubMed]
- Billè A, Okiror L, Karenovics W, et al. Experience with titanium devices for rib fixation and coverage of chest wall defects. Interact Cardiovasc Thorac Surg 2012;15:588-95. [PubMed]
- King RM, Pairolero PC, Trastek VF, et al. Primary chest wall tumors: factors affecting survival. Ann Thorac Surg 1986;41:597-601. [PubMed]
- Gross JL, Younes RN, Haddad FJ, et al. Soft-tissue sarcomas of the chest wall: prognostic factors. Chest 2005;127:902-8. [PubMed]
- Gonfiotti A, Santini PF, Campanacci D, et al. Malignant primary chest-wall tumours: techniques of reconstruction and survival. Eur J Cardiothorac Surg 2010;38:39-45. [PubMed]
- Duranti L, Gronchi A, Stacchiotti S, et al. Localised thoracic sarcomas: outcome improvement over time at a single institution. Eur J Cancer 2013;49:2689-97. [PubMed]
- Kachroo P, Pak PS, Sandha HS, et al. Single-institution, multidisciplinary experience with surgical resection of primary chest wall sarcomas. J Thorac Oncol 2012;7:552-8. [PubMed]


