Patient safety in thoracic surgery and European Society of Thoracic Surgeons checklist
Introduction
An “adverse event” can be defined as any injury due to the medical care. They represent a major source of morbidity and mortality. It is surprising that, only during the twentieth century, clinicians, as a group, thought about “curing and not harming” as an innovative approach to medicine (1). The concept of avoiding patient harm was already stated in the Hippocratic Oath (2). Although this oath is not recognized in many countries of the world and has been modified on several occasions along history, the principle of “do no harm” is considered a basic ethical principle of our profession. Benefits always should outweigh any possible damage induced by the treatment (3).
Since the eighteen century, some important individual initiatives were dismissed (4). The most important difference with today’s point of view is that the whole community agrees on the need to implement efforts protecting our patients. In the past, many initiatives were misunderstood by the medical community. As a result, some of the pioneers were isolated from social recognition and the proposed initiative was not implemented at that time. More recently, the importance of this ethical principle has grown progressively as quality of performance was measured.
Patient safety goes one step forward so it can be defined as the avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of healthcare. From a practical point of view, in most settings, this has to do with anticipating and reacting properly to an unexpected situation or problem. But patient safety is more because it is in charge of determining what is unacceptable to deliver better care (5).
The purpose of this paper is to review briefly what we know about patient harm, what we are working on to protect individual safety within the surgical field and to present a specific initiative: the ESTS checklist.
Patient harm: size matters
Fourteen years after the American report (1), many papers and reports had been published presenting the figures about the incidence and the impact of patient harm (6-11). What is common to all of them is the size of these figures. de Vries et al., performed a systematic review about the incidence of in-hospital adverse effects and found that 1 out of 10 patients will suffer an adverse effect when receiving hospital care (7). According to a report published in 2008 (12), the WHO estimates that 7.5% to 10.4% of patients in acute care settings, in developed countries, experience an adverse drug event that results in 140,000 deaths annually in the USA alone. These adverse drug events affect the elderly especially with an estimation rate of 50 errors per 1,000 person-year in the USA. At least, 27% of these events are considered to be preventable. Data, also suggest, a rate of 6.3 adverse effects per 1,000 patient-days due to medical device problems within developed countries. The size of this problem can be magnified in the developing countries where medical equipment is often useless owing to the lack of resources. Up to 1 out of 4 patients, admitted to the Intensive Care Units in the world, will acquire an infection during the hospital stay. This infection will have an additional cost of US$7-8.2 billion annually in the USA to €800 million in the United Kingdom and France or US$48 million in Turkey.
This sparse data gives a global idea of the magnitude of what patient harm means. Preventable medical errors cost a large amount of money and they produce an enormous personal cost not only in human lives but also in disability, loss of personal satisfaction and loss of general faith in the health care system (13). They have medical, legal, social and emotional implications.
Safety management: why measure
Safety management is related to a broad variety of activities that have to do with all aspects of healthcare itself and includes activities not only from caregivers but from policymakers, regulators and patients.
Since the beginning of global interest in patient safety, a lot of research has been dedicated to develop wide-ranging systems for measurement and monitoring safety issues. This is a difficult task because it has to include data and details from a broad spectrum of areas. There is no doubt that improving patient safety culture and climate decreases patient harm as it has been demonstrated worldwide reducing the number of catheter bloodstream infections as a result of local, evidence-based initiatives (14) among others but still there is a long way to go.
From other high risk industries such as nuclear, aviation, food management or oil manufacturing we have learnt that information of safety alone is of little use. Patient safety needs an organized broad approach which is referred to as safety management system (SMS) (15). SMS receives and combines data from leading an minor indicators to measure, monitor and manage safety performance constantly (15). SMS is composed of policies, structural elements, strategies, means to measure and review safety performance and feedback for final improvement. Although a great part of what we have now has evolved directly from other industries; developed tools, methods and techniques of these industries cannot always be applied to the health care system so further research is necessary.
As it is inferred, measurement should be used to understand, detect and improve. It is a means to an end not the end in itself. But the real difficulty is measuring what really matters. What are the most appropriate metrics to measure? At present there are not clear protocols to evaluate whether safety efforts are reducing the risk of events that cannot be measured as rates (16). Root cause analysis, global trigger tool, patient thermometer, safety case discussions and simple regular morbidity and mortality rounds, for example, are well described tools for understanding, monitoring and evaluating patient safety (17).
Surgical preventable errors: a major concern
It is estimated that 234 million operations are performed globally each year (18). In industrialized countries major complications are reported to occur in 3% to 6% of inpatient surgical procedures, with permanent disability or death rates of 0.4% to 0.8%. The WHO estimates that surgical adverse events account for 48% of all adverse events recorded and affect about 2% of all hospitalized patients (12) and, what is more important, 50% of them are considered to be preventable (8,19).
The delivery of safe effective surgical care is complex (20). Adverse events can occur almost in any step of the health care procedure and are due most to faulty systems, processes and conditions that lead people to make mistakes or fail to prevent them (1). In 1990, Caplan et al. (21), published that respiratory events were responsible for 34% of all anesthetist claims in the US. Eighty-five percent of this adverse events ending in death or in cerebral damage, 72% of the problems were considered preventable simply by improving monitoring. For example, esophageal intubation was responsible for the negative outcome in 18% of the cases. In almost half of these cases, unfortunate auscultation of breath sounds did not identify the cause of the inadequate ventilation. The general spread of a new technique raises a general concern about safety compared to previous methods so prospective comparative studies for safety assessment should be conducted (22).
There are a special group of negative outcomes: wrong-site, wrong procedure and wrong patient operations are the “never events” group (23). This group encompasses one of the most unacceptable medical errors. Of great concern were the data presented by Kwaan et al. (24), that found that wrong-site non-spine procedures were infrequent (1 every 112,994) but protocols used to control this adverse event might have prevented only 62% of the cases of such unacceptable outcome. When assessing the place where the first error took place, they found that 9 out of 13 patients were wrongly assigned preoperatively. The absence of specific protocols preclude that the previous errors were corrected and the harm prevented. There are a certain number of well recognized risk factors for never events outcomes. For example: several surgeons involved in one procedure or multiple procedures for one type of operation, time pressure, emergency surgery, abnormal patient anatomy or morbid obesity (25). Not all specialties have the same risk being orthopedics surgery one with the highest risk of all (26) and being extremely rare in the general thoracic settings (27).
Safe surgery saves lives: the World Health Organization initiative
Probably one of the key points in patient safety is anticipation of possible problems. Anticipation and preparedness are critical components of safety. The importance of these elements is well stressed in other high-risk areas like emergency interventions as in case of fire (28). In surgery as well in all these high-risk areas, another important point should be emphasized: teamwork (29-31). Teamwork is based on communication. The better it is, the better the results will be. Different aspects of communication such as assertiveness, team decision making and team briefing are basic requisites that need training in order to achieve the proposed change in safety attitudes of the team (32). It has been verified that systematic use of checklists improves all this aspects (33).
In 2007, the WHO launched the program call Safe Surgery Saves Lives attempting to achieve a reduction in the number of preventable surgical errors based on a three stage surgical checklist (34). Based on an extensive review of epidemiological data organized to prioritize which were the most important topics that contribute to unsafe care within the surgical field, the group proposed a checklist that includes details that try to overcome the gaps between in-charge teams and different stages of the procedure. A great effort of preparedness and anticipation is summarized in this checklist. Another important aspect, regarding the effectiveness of the checklist is how the cross check is carried out. Different videos are available for proper training. Another relevant issue about surgical checklist is that they are effective. An interesting study has been performed using a stepped wedge cluster randomize controlled methodology that shows that the progressive introduction of the checklist, after adjusting for different confounding factors, decreased significantly the in-hospital mortality (35).
The European Association of Cardiothoracic Surgery (EACTS) in 2012 reviewed relevant and available evidences and recommendations in order to design specific checklists (36). They designed documents for thoracic and cardiac procedures and one common for cardiopulmonary transplant. Checklists are simple and easy to use. The thoracic one includes few implementations over the one proposed by the WHO (33).
A new tool: the ESTS checklist
Soon after the creation of the quality of life and patient safety committee in the society, a limited an informal questionnaire was launched to the different country representatives within the society in order to know the degree of interest and implementation of safety initiatives in each county. From the answers, it was inferred that western European countries were already working and implementing different safety initiatives. But at that moment, in some eastern European countries, safety culture was not a priority.
The WHO checklist (34) is a basic, wide range document developed to fit in any surgical case in any settings all around the world. Thoracic surgeons are working in very complex units and performing very complex procedures that need the highest quality of safety to achieve the best possible results. Then, we wanted to create a checklist that fitted the high requirements these complex procedures are demanding. Using the three stages format, we developed a new checklist (Figure 1) making more emphasis in accurate preparation of the patient (before induction on anesthesia). It is true that problems can appear also during the intraoperative period and after leaving the operating room, specially, because communication between successive teams may fail. During discussion, it was considered that the items already present at the WHO checklist were precise enough and needed no change. Furthermore, increasing the awareness at the beginning of the procedure makes the whole process safer. Future analysis will agree or not with this statement.
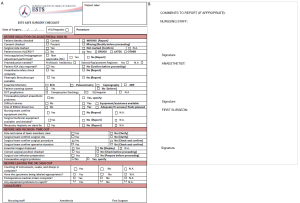
As it was commented before, a great part of the problems are related to a wrong preoperative evaluation or assignation (24). Many of these problems, if detected, can be solved before proceeding. This was one of the main ideas when designing the document: if anybody during the crosschecking process detects a standard deviation, he or she has to know what to do next. Here, in every item, when a problem is detected, a short command will tell the person in charge how to proceed. Sometimes the command is to report the problem. This is another utility of this document: being an onsite reporting system (Figure 1B) to collect information from simple incidents to near-misses (without harm) or accidents (with harm). It can be argued that reporting systems are recommended to be confidential and voluntary but having real time prospective data will increase the quality of these notifications.
Finally, it is important to stress the fact that the ESTS checklist has been translated to 10 different languages in order to provide a ready to download document to those surgeons that need it. As more new languages are enrolled within the society more translations will be provided.
In conclusion, patient safety is becoming an important area of research and improvement to offer the best quality of care as possible. The ESTS checklist integrates the basic values introduced by the WHO to perform the preoperative cross check and introduces several innovations. These innovations are mainly related to several aspects of the preoperative allocation and preparation of the patient and try to anticipate and avoid some of the mistakes detected in previous works on this topic.
Acknowledgements
The author wishes to acknowledge the collaboration of Cecilia Pompili and Bram Balduyck, as members of the ESTS Quality Of Life and Safety Patient committee, for their participation in the development of the survey mentioned in this paper, the discussion of its results and their contributions to the successive versions of the ESTS developed checklist.
Disclosure: The author declares no conflict of interest.
References
- Kohn LT, Corrigan JM, Donaldson MS. eds. To Err Is Human: Building a Safer Health System. Washington: National Academies Press, 2000.
- Emery AE. Hippocrates and the oath. J Med Biogr 2013;21:198-9. [PubMed]
- Sokol DK. “First do no harm” revisited. BMJ 2013;347:f6426. [PubMed]
- Health Foundation: Patient safety timeline. Available online: https://prezi.com/m6sautyrz4a6/health-foundation-patient-safety-timeline, accessed on December 10, 2014.
- Vincent C. eds. Patient Safety. Singapore: John Wiley & Sons, 2011.
- Baker GR, Norton PG, Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678-86. [PubMed]
- de Vries EN, Ramrattan MA, Smorenburg SM, et al. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care 2008;17:216-23. [PubMed]
- Kable AK, Gibberd RW, Spigelman AD. Adverse events in surgical patients in Australia. Int J Qual Health Care 2002;14:269-76. [PubMed]
- Kunac DL, Kennedy J, Austin N, et al. Incidence, preventability, and impact of Adverse Drug Events (ADEs) and potential ADEs in hospitalized children in New Zealand: a prospective observational cohort study. Paediatr Drugs 2009;11:153-60. [PubMed]
- Thomsen LA, Winterstein AG, Søndergaard B, et al. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother 2007;41:1411-26. [PubMed]
- Vlayen A, Verelst S, Bekkering GE, et al. Incidence and preventability of adverse events requiring intensive care admission: a systematic review. J Eval Clin Pract 2012;18:485-97. [PubMed]
- Jha AK. eds. Summary of the Evidence on Patient Safety: Implications for Research. Switzerland: World Health Organization, 2008.
- Massó Guijarro P, Aranaz Andrés JM, Mira JJ, et al. Adverse events in hospitals: the patient’s point of view. Qual Saf Health Care 2010;19:144-7. [PubMed]
- Pronovost P, Needham D, Berenholtz S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725-32. [PubMed]
- Waring A. eds. Safety management systems. London: Chapman & Hall, 1996.
- Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: an elusive target. JAMA 2006;296:696-9. [PubMed]
- Available online: http://patientsafety.health.org.uk/area-of-care/safety-management/measurement-and-analysis. London: The Health Foundation, accessed on November 28th, 2014.
- Available online: www.npsa.nhs.uk/advice, accessed on December 20th, 2014.
- 10 Facts On Patient Safety. WHO. Available online: http://www.who.int/features/factfiles/patient_safety/patient_safety_facts/en/index2.html, accessed on November 21st, 2014.
- Vincent C, Moorthy K, Sarker SK, et al. Systems approaches to surgical quality and safety: from concept to measurement. Ann Surg 2004;239:475-82. [PubMed]
- Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology 1990;72:828-33. [PubMed]
- Zeltsman D. Current readings: Redefining minimally invasive: uniportal video-assisted thoracic surgery. Semin Thorac Cardiovasc Surg 2014;26:249-54. [PubMed]
- Michaels RK, Makary MA, Dahab Y, et al. Achieving the National Quality Forum’s “Never Events”: prevention of wrong site, wrong procedure, and wrong patient operations. Ann Surg 2007;245:526-32. [PubMed]
- Kwaan MR, Studdert DM, Zinner MJ, et al. Incidence, patterns, and prevention of wrong-site surgery. Arch Surg 2006;141:353-7; discussion 357-8. [PubMed]
- Shojania KG, Duncan BW, McDonald KM, et al. Making health care safer: a critical analysis of patient safety practices. Evid Rep Technol Assess (Summ) 2001;43:i-x,1-668. [PubMed]
- Cowell HR. Wrong-site surgery. J Bone Joint Surg Am 1998;80:463. [PubMed]
- Cassivi SD, Allen MS, Vanderwaerdt GD, et al. Patient-centered quality indicators for pulmonary resection. Ann Thorac Surg 2008;86:927-32. [PubMed]
- Wang B, Li H, Rezgui Y, et al. BIM based virtual environment for fire emergency evacuation. ScientificWorldJournal 2014;2014:589016.
- Salas E, Wilson KA, Burke CS, et al. Does crew resource management training work? An update, an extension, and some critical needs. Hum Factors 2006;48:392-412. [PubMed]
- Wallin CJ, Meurling L, Hedman L, et al. Target-focused medical emergency team training using a human patient simulator: effects on behaviour and attitude. Med Educ 2007;41:173-80. [PubMed]
- Wiegmann DA, Shappell SA. Human error and crew resource management failures in Naval aviation mishaps: a review of U.S. Naval Safety Center data, 1990-96. Aviat Space Environ Med 1999;70:1147-51. [PubMed]
- Grogan EL, Stiles RA, France DJ, et al. The impact of aviation-based teamwork training on the attitudes of health-care professionals. J Am Coll Surg 2004;199:843-8. [PubMed]
- Russ S, Rout S, Sevdalis N, et al. Do safety checklists improve teamwork and communication in the operating room? A systematic review. Ann Surg 2013;258:856-71. [PubMed]
- World Health Organization. eds. World Alliance for Patient Safety: WHO Guidelines on Hand Hygiene in Health Care: a Summary. Geneva: World Health Organization, 2005.
- Haugen AS, Søfteland E, Almeland SK, et al. Effect of the World Health Organization Checklist on Patient Outcomes: A Stepped Wedge Cluster Randomized Controlled Trial. Ann Surg 2014. [Epub ahead of print]. [PubMed]
- Clark SC, Dunning J, Alfieri OR, et al. EACTS guidelines for the use of patient safety checklists. Eur J Cardiothorac Surg 2012;41:993-1004. [PubMed]


