Correlation between familial cancer history and epidermal growth factor receptor mutations in Taiwanese never smokers with non-small cell lung cancer: a case-control study
Introduction
Lung cancer is a leading cause of cancer deaths worldwide with more than one million deaths each year (1). Patients often present with advanced disease at diagnosis and are ineligible for curative treatment (2). Despite advances in therapy, prognosis has been poor with 5-year survival rates of 16% for affected patients (3). Cigarette smoking remains a prominent risk factor for developing lung cancer and accounts for the majority of cancer deaths (4). Consequently, previous research has focused on lung cancer in cigarette smokers.
However, lung cancer incidence has been increasing in never smokers (5). Never smokers now constitute nearly 25% of lung cancer patients worldwide, a trend that is especially prominent in Asia, where 50% of women with lung cancer never smoke (6,7). Risk factors other than tobacco contribute to cancer development, including occupational carcinogens, air pollution, cooking fumes, and genetic abnormalities (8). Previous studies have linked specific genetic abnormalities to lung cancer development (9-11).
Furthermore, lung cancer patients often reported first degree relatives with cancer, reflecting potential genetic factors associated with carcinogenesis (12). Although definite evidence of heritable genetic mutations remains elusive, familial aggregations of lung cancer patients with epidermal growth factor receptor (EGFR) mutations have been documented (13). A previous investigation of EGFR mutations and familial cancer history in lung cancer patients reported an insignificant association, but the cohort mainly involved Caucasians who were less susceptible to EGFR mutations (14). Since Asians and Caucasians with lung cancer have different prevalence of EGFR mutations, the relationship between familial cancer history and EGFR mutations in these ethnic groups may differ (15). This study aims to clarify the correlation between familial cancer history and the prevalence of EGFR mutations in Taiwanese never smokers with lung cancer.
Patients and methods
Patient selection
Never smokers with lung cancer treated at a tertiary hospital in Taiwan from April 2012 to May 2014 were evaluated for eligibility. Inclusion criteria were never smokers, defined by a lifetime use of less than 100 cigarettes, with a diagnosis of non-small cell lung cancer (NSCLC). Patients must have records of tumor genotype and familial cancer history for inclusion. Tumor samples were obtained by bronchoscopic or image guided biopsy and subsequently genotyped using direct polymerase chain reaction-based EGFR mutation tests. Exclusion criteria involved patients without records of familial cancer history or tumor genotype. The authors’ institution does not require review of retrospective studies involving de-identified medical records.
Data collection
Data including age, gender, disease stage, histology, tumor genotype, and familial cancer history were collected from medical records. Lung cancer patients with familial cancer history were allocated to cases, while lung cancer patients without family history were designated as controls. Familial cancer history was positive if any first or second degree relative had a diagnosis of cancer. However, due to the retrospective nature of family history collection, further sub-classification of familial heritage was not feasible. The study outcome was the prevalence of EGFR mutations in lung cancer patients with familial cancer history compared to those without family history. Patients with familial cancer history were further divided into those with family history of lung cancer and those with family history of non-pulmonary cancers. Finally, in the subset of patients with familial cancer history, the correlation between EGFR mutations and selected clinical characteristics was investigated.
Statistical analysis
Demographic characteristics of cases and controls were compared using Pearson’s chi-squared test for categorical variables and t-test for continuous variables. Pearson’s chi-squared test extrapolated the correlation between familial cancer history and EGFR mutations in lung cancer patients. Cross tabulation enabled calculations of odds ratio (OR) and 95% confidence interval (CI). All P values were based on a two-sided hypothesis. Analyses were performed using International Business Machines Statistical Package for the Social Sciences version 20 (SPSS Inc. Chicago, USA).
Results
Description of subjects
This study assessed 246 never smokers with lung cancer for eligibility. All patients had records of tumor genotype and familial cancer history, and therefore no exclusion of subjects occurred during analysis.
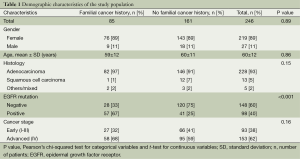
Demographic characteristics of cases and controls are shown in Table 1. Baseline characteristics including age, gender, disease stage, and histology showed no statistically significant difference between groups. The study population mainly involved never smoking women with a mean age of 60 years, and the predominant tumor histology was adenocarcinoma. The overall prevalence of EGFR mutations was 98 out of 246 patients (40%).
Full table
Familial cancer history and EGFR mutations
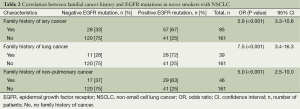
Lung cancer patients with familial cancer history had an increased prevalence of EGFR mutations compared to patients without family history (OR: 5.9; 95% CI: 3.3-10.6; P<0.001). Specifically, 57 out of 85 lung cancer patients (67%) with familial cancer history harbored EGFR mutations, while 41 out of 161 cancer patients (25%) without family history had these mutations. Table 2 summarizes these findings.
Full table
Family history of lung cancer and EGFR mutations
Patients reporting family history specifically of lung cancer had higher prevalence of EGFR mutations compared to patients without familial cancer history (OR: 7.5; 95% CI: 3.4-16.3; P<0.001). Specifically, 28 out of 39 cancer patients (72%) with family history of lung cancer carried EGFR mutations, while 41 out of 161 patients (25%) without familial cancer history harbored these mutations. Importantly, there was a stronger association between EGFR mutations and familial lung cancer history compared to family history of any cancer. These observations are presented in Table 2.
Family history of non-pulmonary cancers and EGFR mutations
Lung cancer patients with family history of non-pulmonary cancers had an increased prevalence of EGFR mutations compared to patients without family history (OR: 5.0; 95% CI: 2.5-10.0; P<0.001). Specifically, 29 out of 46 cancer patients (63%) with family history of non-pulmonary cancers harbored EGFR mutations, whereas 41 out of 161 patients (25%) without any familial cancer history carried these mutations. The findings are presented in Table 2.
Familial cancer history and clinical characteristics
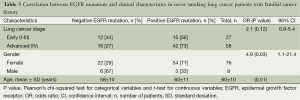
In the subset of patients with familial cancer history, those with EGFR mutations were associated with advanced stage IV disease (OR: 2.1; 95% CI: 0.8-5.4; P=0.12), although the trend did not achieve statistical significance. Lung cancer patients with EGFR mutations were more frequently female (OR: 4.9; 95% CI: 1.1-21.4; P=0.03), while no difference in age was observed regardless of EGFR mutation status. These findings are presented in Table 3.
Full table
Discussion
Epidemiological studies have consistently demonstrated that familial cancer history increases the risk of developing lung cancer (16,17), which suggests potentially heritable genetic factors in cancer development. Indeed, heritable susceptibility mutations have been identified on chromosome 6q and EGFR-T790M in familial aggregations of lung cancer patients (18,19). Asians in particular have increased susceptibility to EGFR mutations due to a combination of polymorphisms, mutations, and amplifications, and these mutations are well documented in the pathogenesis of lung cancer (20). Therefore, Asians with lung cancer may better reflect the relationship between familial cancer history and EGFR mutations.
This study demonstrated an increased prevalence of EGFR mutations in never smoking lung cancer patients with familial cancer history. These mutations contribute to lung cancer development and may explain the strong association between family history and lung cancer risk in Asian never smokers (21). The study also revealed that a sizable proportion (40%) of lung cancer patients in Taiwan harbored EGFR mutations, compared to a lower prevalence (10-15%) reported in Caucasians (22). Several implications arise from these observations.
An increased prevalence of EGFR mutations in Asians with lung cancer implies that more patients may respond to tyrosine kinase inhibitors (TKI). Overall, TKI yielded favorable clinical response in lung cancer patients with EGFR mutations (23). TKI also significantly delayed disease progression in patients with advanced cancer (24). As shown in this study, lung cancer patients with familial cancer history commonly harbored EGFR mutations and may therefore benefit from TKI therapy. For instance, patients with familial cancer history suffering from life threatening conditions such as brain metastasis should be considered for empirical TKI treatment. Of course, these patients should eventually receive EGFR mutation analysis to justify TKI therapy.
A family history specifically of lung cancer was found to increase the prevalence of EGFR mutations in never smokers with lung cancer. This finding emphasizes the role of genetic abnormalities in lung cancer development. Due to the observed familial aggregation of lung cancer patients, family members of never smoking patients with EGFR mutations may have a genetic predisposition to lung cancer development and should receive appropriate screening study. Interestingly, this study also observed a significant association between EGFR mutations and family history of non-pulmonary cancers, although the association was stronger in patients with familial lung cancer history. Family history of non-pulmonary cancers may affect the prevalence of EGFR mutations in never smokers with lung cancer because a number of different tumors such as squamous carcinomas have also been associated with these mutations (25). Of course, EGFR mutations in lung cancer and non-pulmonary cancers may occur at different genetic loci, and the role of EGFR mutations in different cancers requires further investigation.
Analysis of patients with concomitant familial cancer history and EGFR mutations showed a tendency towards more advanced disease at diagnosis. This reinforces the previous finding that patients with familial lung cancer history frequently experienced worse clinical outcome than those without family history (26). A possible explanation may lie in the oncogenic effects of EGFR mutations on lung cancer cells, including promotion of cancer proliferation, angiogenesis and metastasis (27). Since patients with positive familial cancer history were also shown to have higher prevalence of EGFR mutations, they should receive more comprehensive survey at diagnosis to identify evidence of advanced disease.
Never smokers with lung cancer were frequently women in this study, which is compatible with previous literature (28). That Asian women were less likely to smoke partly explained their increased representation in never smokers with lung cancer, but hormonal factors and cooking practice also contributed to cancer development in this population (29-31). Specifically, estrogen receptors may interact with EGFR in the pathogenesis of cancer in women (32).
The study provides novel information by examining a homogenous cohort of Taiwanese never smokers with lung cancer. Since cigarette smoking is an independent risk factor for developing lung cancer, never smokers better reflect the genetic factors associated with cancer development. Furthermore, all study subjects had complete documentation of familial cancer history and tumor genotype. Selection bias was avoided because of similar demographic characteristics between cases and controls. Recall bias was overcome by extracting data from existing medical records.
This study had several limitations. Firstly, environmental exposure was a potential confounding factor. However, since participants resided in the same municipality in central Taiwan, baseline environmental exposure such as air pollution should be comparable. Secondly, since never smoking lung cancer patients in Taiwan were more likely to be women, the study’s results may not be applicable to other populations. Thirdly, further sub-classification of familial cancer history according to degree of consanguinity would allow better understanding of its effects on the prevalence of EGFR mutations in never smoking lung cancer patients.
In conclusion, familial cancer history increased the prevalence of EGFR mutations in Taiwanese never smokers with lung cancer. Lung cancer patients with familial cancer history frequently harbored EGFR mutations and may respond favorably to TKI, and a family history of cancer can guide empirical TKI therapy in patients with life threatening disease. In essence, lung cancer in never smokers may be a distinct entity in which genetic factors play an important role.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Jemal A, Center MM, DeSantis C, et al. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev 2010;19:1893-907. [PubMed]
- Molina JR, Adjei AA, Jett JR. Advances in chemotherapy of non-small cell lung cancer. Chest 2006;130:1211-9. [PubMed]
- Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 2011;61:212-36. [PubMed]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. 2014.
- Boffetta P, Järvholm B, Brennan P, et al. Incidence of lung cancer in a large cohort of non-smoking men from Sweden. Int J Cancer 2001;94:591-3. [PubMed]
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [PubMed]
- Couraud S, Zalcman G, Milleron B, et al. Lung cancer in never smokers--a review. Eur J Cancer 2012;48:1299-311. [PubMed]
- Sun S, Schiller JH, Gazdar AF. Lung cancer in never smokers--a different disease. Nat Rev Cancer 2007;7:778-90. [PubMed]
- Li Y, Sheu CC, Ye Y, et al. Genetic variants and risk of lung cancer in never smokers: a genome-wide association study. Lancet Oncol 2010;11:321-30. [PubMed]
- Brennan P, Hainaut P, Boffetta P. Genetics of lung-cancer susceptibility. Lancet Oncol 2011;12:399-408. [PubMed]
- Cooper WA, Lam DC, O’Toole SA, et al. Molecular biology of lung cancer. J Thorac Dis 2013;5:S479-90. [PubMed]
- Mayne ST, Buenconsejo J, Janerich DT. Familial cancer history and lung cancer risk in United States nonsmoking men and women. Cancer Epidemiol Biomarkers Prev 1999;8:1065-9. [PubMed]
- Pennell NA, Yin L, Keshtgarpour M, et al. Two generations of light/never-smokers with advanced adenocarcinoma of the lung with durable responses to erlotinib. J Thorac Oncol 2012;7:1200-1. [PubMed]
- Gaughan EM, Cryer SK, Yeap BY, et al. Family history of lung cancer in never smokers with non-small-cell lung cancer and its association with tumors harboring EGFR mutations. Lung Cancer 2013;79:193-7. [PubMed]
- Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol 2014;9:154-62. [PubMed]
- Lissowska J, Foretova L, Dabek J, et al. Family history and lung cancer risk: international multicentre case-control study in Eastern and Central Europe and meta-analyses. Cancer Causes Control 2010;21:1091-104. [PubMed]
- Matakidou A, Eisen T, Houlston RS. Systematic review of the relationship between family history and lung cancer risk. Br J Cancer 2005;93:825-33. [PubMed]
- Bailey-Wilson JE, Amos CI, Pinney SM, et al. A major lung cancer susceptibility locus maps to chromosome 6q23-25. Am J Hum Genet 2004;75:460-74. [PubMed]
- Tibaldi C, Giovannetti E, Vasile E, et al. Inherited germline T790M mutation and somatic epidermal growth factor receptor mutations in non-small cell lung cancer patients. J Thorac Oncol 2011;6:395-6. [PubMed]
- Nomura M, Shigematsu H, Li L, et al. Polymorphisms, mutations, and amplification of the EGFR gene in non-small cell lung cancers. PLoS Med 2007;4:e125. [PubMed]
- Nitadori J, Inoue M, Iwasaki M, et al. Association between lung cancer incidence and family history of lung cancer: data from a large-scale population-based cohort study, the JPHC study. Chest 2006;130:968-75. [PubMed]
- Gaughan EM, Costa DB. Genotype-driven therapies for non-small cell lung cancer: focus on EGFR, KRAS and ALK gene abnormalities. Ther Adv Med Oncol 2011;3:113-25. [PubMed]
- Webb S, Thomas M, Metcalf C, et al. EGFR mutation testing in NSCLC: patterns of care and outcomes in Western Australia. Asia-Pacific Journal of Clinical Oncology 2009;5:66-71.
- Wu YL, Chu DT, Han B, et al. Phase III, randomized, open-label, first-line study in Asia of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer: evaluation of patients recruited from mainland China. Asia Pac J Clin Oncol 2012;8:232-43. [PubMed]
- Voldborg BR, Damstrup L, Spang-Thomsen M, et al. Epidermal growth factor receptor (EGFR) and EGFR mutations, function and possible role in clinical trials. Ann Oncol 1997;8:1197-206. [PubMed]
- Ganti AK, Loberiza FR Jr, Kessinger A. Association of positive family history with survival of patients with lung cancer. Lung Cancer 2009;63:136-9. [PubMed]
- Sharma SV, Bell DW, Settleman J, et al. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer 2007;7:169-81. [PubMed]
- Badar F, Meerza F, Khokhar RA, et al. Characteristics of lung cancer patients--the Shaukat Khanum Memorial experience. Asian Pac J Cancer Prev 2006;7:245-8. [PubMed]
- Toh CK, Gao F, Lim WT, et al. Never-smokers with lung cancer: epidemiologic evidence of a distinct disease entity. J Clin Oncol 2006;24:2245-51. [PubMed]
- Yu IT, Chiu YL, Au JS, et al. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Res 2006;66:4961-7. [PubMed]
- Siegfried JM. Women and lung cancer: does oestrogen play a role? Lancet Oncol 2001;2:506-13. [PubMed]
- Levin ER. Bidirectional signaling between the estrogen receptor and the epidermal growth factor receptor. Mol Endocrinol 2003;17:309-17. [PubMed]


