IgG4-related lung disease with atypical CT imaging: a case report
Introduction
IgG4-related disease is a systemic disease, and can involve multiple organs. It is characterized by increased serum level of IgG4, infiltration of IgG4-positive lymphocytes in multiple tissues, and tissue fibrosis (1). There are various organ-specific manifestations such as IgG4-related lung disease, autoimmune pancreatitis, sclerosing cholangitis, sclerosing salivary gland inflammation, inflammatory pseudotumor, interstitial nephritis and retroperitoneal fibrosis (2,3). The incidence of IgG4-related lung disease is 15-54% (4).
Okazaki et al. suggests the following diagnostic criteria of IgG4-related disease: single or multiple organs showing diffuse or limited swelling; an IgG4 level in serum >1.35 g/L; and significant lymphoplasmacytic infiltration on histological assessment (5). Fibrosis and obliterans could also be observed. To make the diagnosis, IgG4-positive plasma cells need to be present at >10 per high power field (HPF), or the ratio of IgG4-positive plasma cells to all IgG plasma cell subtypes needs to be >0.4. While the pathological features of this disorder can vary between patients, the main feature is lymphoplasmacytic infiltration or fibrosis. This in turn leads to a variety of radiological features.
Case report
A 24-year-old woman was hospitalized with recurring cough and fever over a 2 month period, along with shortness of breath for 2 weeks. Physical examination demonstrated no significant abnormalities. Laboratory examination revealed an elevated ESR (105 mm/h) and CRP (28.74 mg/L); the total count of white blood cell (WBC) was increased (11.47×109/L), but the ratio of neutrophilia (70.1%) was increased slightly (close to the normal proportion). Total IgG levels were increased (18.60 g/L), including serum IgG4. Tumour markers including CEA, CA-125, CA-153 and CA-199 were all normal. And autoimmune markers including anti-nuclear antibodies, rheumatoid factor and anti-neutrophil cytoplasmic antibodies were negative, too.
Computed tomography (CT) images demonstrated multiple nodules or masses in both lungs, principally located in the upper lobes (Figure 1A). These varied in size from 0.3 cm × 0.4 cm to 3 cm × 2.7 cm, and had homogeneous density with significant enhancement (33 Hounsfield units for the plain scan compared with 102 HU for the enhanced scan). Importantly, thickened interlobular septa were also observed in the upper lobes (Figure 1B).
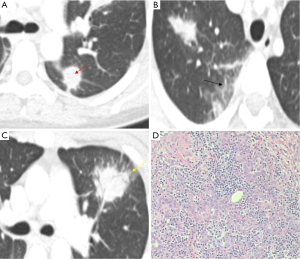
Additional radiological features included the ‘halo sign’ evident around some high-density lesions (Figure 1C), along with irregular edges, massive spiculation and the presence of the vessel convergence sign. Furthermore, some lesions were located peripleurally, with thickened and tractive adjacent pleura. The effusion was observed in the left pleural cavity. Bilateral hilar and mediastinal lymphadenopathy was also evident and enlarged.
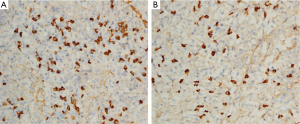
Tissue for pathologic examination was obtained by fiber-optic bronchoscopy. In inspective lung tissue, many inflammatory cells (principally lymphocytes and plasma cells) were observed in pulmonary parenchyma (Figure 1D), accompanied by significant fibrosis. The lymphoplasmacytic infiltration was also observed in the interlobular interstitium, the peribronchiolar region and the alveolar interstitium. Moreover, IgG4-positive plasma cells were present on immunohistochemical staining. In Figure 2A,B, the deep cells were on behalf of IgG4-positive plasma cells (>50/HPF). Immunostaining for CD20, CD3, CD138, CD38, mum-1, CD21FDC and CD23 were all positive; stains for desmin, ALK, SMA and EBER were negative. A histological diagnosis of IgG4-related lung disease was made by the increased serum IgG4 and the tissue’s infiltration of IgG4-positive lymphocytes,
On admission, this case was misdiagnosed as infection, possibly due to atypical bacteria. After anti-inflammatory treatment for 2 weeks, no improvement was evident. Then voriconazole was also used for antifungal therapy. However, the radiological picture worsened with an increase in size of several nodules. Following histological diagnosis, the management was converted to hormonal therapy, with a significant improvement in clinical and radiological abnormalities being observed over a 2-month period.
Discussion
CT findings
The CT findings in this case are various and atypical, and some findings differ from those reported in the current literature. Inoue et al. (6) collected 13 cases of IgG4-related lung disease, and reported that it could be categorized into four major subtypes: (I) the solid nodular type, where a solitary nodular mass lesion was present (four cases); (II) the round ground-glass opacity (GGO) type, characterized by multiple round GGOs (two cases); (III) the alveolar interstitial type, with honeycombing, bronchiectasis, and diffuse GGO (two cases); and (IV) the bronchovascular type, where there was thickening of bronchovascular bundles and interlobular septa (five cases). Histological review demonstrated that the solitary nodular lesions consisted of diffuse lymphoplasmacytic infiltration and fibrosis in pulmonary parenchyma. Thickened bronchovascular bundles or interlobular septa and GGO on CT images corresponded at a histological level to lymphoplasmacytic infiltration and fibrosis in peribronchiolar or interlobular interstitium and alveolar interstitium, respectively. In the late stages, the radiological finding of honeycombing corresponded to disrupted alveolar structures and dilated peripleural air spaces.
Importantly, nodules or masses, and thickened interlobular septa are observed concurrently in our case described above. Our case, with its various radiological features, is different from the previously reported cases and could be defined as a hybrid type of IgG4-related lung disease. We could anticipate that these features would be accompanied at the histological level by fibrosis and abundant lymphoplasmacytic infiltration in the pulmonary parenchyma, peribronchiolar, interlobular interstitium and alveolar interstitium.
Matsui et al. reported 18 cases with IgG4-related lung disease, in which the major CT features included thickening of the bronchial wall, bronchovascular bundles and interlobular septa (7). Soft tissue masses were observed only in two cases, suggesting that the majority of these cases belonged to the bronchovascular interstitial type. But in our case, the nodules or masses are more than simply thickened interlobular septa, requiring the creation of a hybrid class of IgG4-related lung disease.
Additional radiological features of this case include the ‘halo sign’ around high-density nodules or masses. The radiologic density of the halo sign is similar to that of GGO, but the distribution of these two features is quite distinct. The haloes surround nodules or masses, while GGO are observed independent of these lesions. Furthermore, the nodules or masses of IgG4-related lung disease always locate in a peripleural position. The adjacent pleura around such lesions may show mild bilateral pleural thickening (8), consistent with the findings in this case.
The bilateral hilar and mediastinal lymphadenopathy in our case is similar to that observed by Matsui. Matsui et al. reported the lymphadenopathy in all 18 patients of their series, using the mediastinal window setting (7). Indeed, mediastinal and/or hilar lymphadenopathy may be the most common intrathoracic manifestation of IgG4-related lung disease, being described in 40-90% of patients (9-11).
The existence of pleural effusions in IgG4-related lung disease is more contentious. Inoue et al. reported no pleural effusions in their 13 cases (6). But the left pleural effusion was observed in our case. The pleural effusion had also been reported by Choi et al. in a patient with IgG4-related lung disease (12). To clarify the significance of effusions in IgG4-related lung disease, a larger case series is required.
Clinical findings
According to the presented references, IgG4 related disease could be common in men of middle and old age. However, as a newly recognized disease, IgG4-related lung disease has not yet been well understood. Up to now, only limited cases have been reported in literature and there are not enough cases to show its all characteristics. Furthermore, Deshpande et al. also reported that young patient and female patient could have IgG4 related disease (13). Moreover, we observe the symptoms of fever in our case, with the increased WBC, CPR and ESR. This situation could exist in IgG4-related disease, as some references reported the similar discoveries (14-16).
On admission, this case was misdiagnosed as infection. At first, the patient accepted anti-inflammatory therapy, which included mezlocillin/sulbactam, azithromycin, moxalactam and imipenem/cilastatin. Then voriconazole was also used for antifungal therapy. However, the radiological picture worsened with an increase in size of several nodules. According to the histological diagnosis of IgG4-related lung disease, the management was converted to corticosteroid therapy. Although experience with treatment regimens in IgG4-related disease was growing, glucocorticoids still appeared to be effective (17). So methylprednisolone (40 mg qd) was used and then the symptoms of fever reduced gradually. The lesions of CT images were absorbed gradually, too. This indicated that the hormone therapy was effective.
Differential diagnosis
IgG4-related lung disease need be identified with Castleman’s disease (plasma cell type) and pulmonary hyalinizing granulomas. These diseases both could have perilymphatic involvement and show abundant IgG4 positive plasma cell infiltration. CT images and clinical findings are important, as they could provide some differential points.
To patients with Castleman’s disease (plasma cell type), the thoracic CT images usually show the enlargement of mediastinal and hilar lymph nodes. Only few study reported that Castleman’s disease (plasma cell type) had perilymphatic involvement and thickened interlobular septa (18,19). This situation is common in IgG4-related lung disease, which is different from Castleman’s disease. Furthermore, multicentric Castleman’s disease could also have elevated serum IgG4 levels. But laboratory findings of anemia, hypoalbuminemia, polyclonal gammaglobulinemia, high C-reactive protein level, and elevated serum interleukin-6 level were all consistent with the multicentric Castleman’s disease (20).
Pulmonary hyalinizing granuloma is a rare and benign disease. Although this disease had various degrees of lymphocytic infiltration within the lesions, its CT images presented as a solitary or, more frequently, multiple pulmonary nodular lesions (21). But IgG4-related lung disease could have different lesions, including the solid nodular mass, the round GGO and the thickened interlobular septa. Moreover, some investigation demonstrated both elevated serum IgG4 and elevated tissue IgG4-positive plasma cells in the pulmonary hyalinizing granuloma (22,23). The morphologic features of pulmonary hyalinizing granuloma overlapped those characteristics in IgG4-related lung disease, which suggested that pulmonary hyalinizing granuloma may be a form of IgG4-related disease.
Conclusions
IgG4-related disease is an uncommon but increasingly reported disease. The lung is well described as a target organ of IgG4-related disease, and the radiologic and pathologic features are varied. This report highlights the need for consideration of this condition even in the context of diverse and atypical features on CT imaging.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med 2012;366:539-51. [PubMed]
- Takahashi H, Yamamoto M, Suzuki C, et al. The birthday of a new syndrome: IgG4-related diseases constitute a clinical entity. Autoimmun Rev 2010;9:591-4. [PubMed]
- Takahashi H, Yamamoto M, Tabeya T, et al. The immunobiology and clinical characteristics of IgG4 related diseases. J Autoimmun 2012;39:93-6. [PubMed]
- Ryu JH, Sekiguchi H, Yi ES. Pulmonary manifestations of immunoglobulin G4-related sclerosing disease. Eur Respir J 2012;39:180-6. [PubMed]
- Okazaki K, Uchida K, Koyabu M, et al. Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. J Gastroenterol 2011;46:277-88. [PubMed]
- Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related lung disease: CT findings with pathologic correlations. Radiology 2009;251:260-70. [PubMed]
- Matsui S, Hebisawa A, Sakai F, et al. Immunoglobulin G4-related lung disease: clinicoradiological and pathological features. Respirology 2013;18:480-7. [PubMed]
- Ryu JH, Sekiguchi H, Yi ES. Pulmonary manifestations of immunoglobulin G4-related sclerosing disease. Eur Respir J 2012;39:180-6. [PubMed]
- Fujinaga Y, Kadoya M, Kawa S, et al. Characteristic findings in images of extra-pancreatic lesions associated with autoimmune pancreatitis. Eur J Radiol 2010;76:228-38. [PubMed]
- Cheuk W, Yuen HK, Chu SY, et al. Lymphadenopathy of IgG4-related sclerosing disease. Am J Surg Pathol 2008;32:671-81. [PubMed]
- Zen Y, Inoue D, Kitao A, et al. IgG4-related lung and pleural disease: a clinicopathologic study of 21 cases. Am J Surg Pathol 2009;33:1886-93. [PubMed]
- Choi JH, Sim JK, Oh JY, et al. A Case of IgG4-Related Disease Presenting as Massive Pleural Effusion and Thrombophlebitis. Tuberc Respir Dis (Seoul) 2014;76:179-83. [PubMed]
- Deshpande V, Khosroshahi A, Nielsen GP, et al. Eosinophilic angiocentric fibrosis is a form of IgG4-related systemic disease. Am J Surg Pathol 2011;35:701-6. [PubMed]
- Sun X, Peng M, Hou X, et al. Refractory IgG4-related lung disease with constitutional symptoms and severe inflammation. Am J Respir Crit Care Med 2014;189:374-5. [PubMed]
- Kobayashi H, Shimokawaji T, Kanoh S, et al. IgG4-positive pulmonary disease. J Thorac Imaging 2007;22:360-2. [PubMed]
- Tsuboi H, Inokuma S, Setoguchi K, et al. Inflammatory pseudotumors in multiple organs associated with elevated serum IgG4 level: recovery by only a small replacement dose of steroid. Intern Med 2008;47:1139-42. [PubMed]
- Stone JH. IgG4-related disease: nomenclature, clinical features, and treatment. Semin Diagn Pathol 2012;29:177-90. [PubMed]
- Iyonaga K, Ichikado K, Muranaka H, et al. Multicentric Castleman's disease manifesting in the lung: clinical, radiographic, and pathologic findings and successful treatment with corticosteroid and cyclophosphamide. Intern Med 2003;42:182-6. [PubMed]
- Murinello N, Matos C, Nogueira F. Castleman's disease: an unusual presentation. J Bras Pneumol 2011;37:129-32. [PubMed]
- Takeuchi M, Sato Y, Takata K, et al. Cutaneous multicentric Castleman's disease mimicking IgG4-related disease. Pathol Res Pract 2012;208:746-9. [PubMed]
- Shibata Y, Kobayashi T, Hattori Y, et al. High-resolution CT findings in pulmonary hyalinizing granuloma. J Thorac Imaging 2007;22:374-7. [PubMed]
- Chapman EM, Gown A, Mazziotta R, et al. Pulmonary hyalinizing granuloma with associated elevation in serum and tissue IgG4 occurring in a patient with a history of sarcoidosis. Am J Surg Pathol 2012;36:774-8. [PubMed]
- Shinohara T, Kaneko T, Miyazawa N, et al. Pulmonary hyalinizing granuloma with laryngeal and subcutaneous involvement: report of a case successfully treated with glucocorticoids. Intern Med 2004;43:69-73. [PubMed]


