Uniportal video assisted thoracoscopic lobectomy: primary experience from an Eastern center
Introduction
The safety and feasibility of video-assisted thoracic surgery (VATS) procedure was well proved since its first application in the early 90s (1,2). While the number of VATS was increasing, a less invasive surgery using decreased number of trocars was demanded. Bases on the accumulated surgical experience and the technical innovation, uniportal VATS was pioneered in some experienced hands from the western countries (3).
Since the first report on uniportal thoracic surgery by Rocco in 2004 (4), the topics on pneumothorax, pleural biopsy, and lung wedge resection using uniportal VATS have shown promising results (5-7). In 2011, Gonzalez-Rivas et al. reported their experience of uniportal thoracoscopic lobectomy, the first worldwide published study on major lung resection (8). But there were few articles about uniportal thoracoscopic major lung resection, and less was known if its application in eastern centers would benefit on patients as well.
Based on our primary experience from uniportal VATS biopsy, we summarize our primary experience on uniportal VATS lobectomy, and evaluate the safety and efficacy of this demanding procedure in this single center.
Materials and methods
The study was approved by the institutional review board and the ethics committee of Zhongshan Hospital of Fudan University. Pre-operative examination including EKG, pulmonary function, chest CT scan, bronchoscope, and brain MRI were administered to exclude the candidates for curative surgery for NSCLC patients.
The inclusion criteria for uniportal VATS lobectomy were as follows:
- Patients with clinically staged T1-3N0M0 tumors;
- Patients without previous history of cancer;
- Patients without previous history of chest surgery;
- Patients with an ASA score of I-II.
The exclusion criteria for uniportal VATS lobectomy were as follows:
- Patients with preexisting tuberculosis/asthma/interstitial lung disease;
- Patients with cardiac, hepatic or renal dysfunction;
- Patients underwent neo-adjuvant therapy.
Clinical features including age, sex, comorbidity, BMI, operation duration, estimated volume of blood loss, morbidity and mortality were recorded in the database (Table 1).
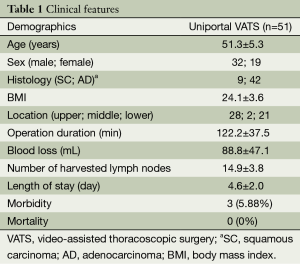
Full table
Anesthesia and analgesia
All patients received a combination of epidural and general anesthesia, and were provided with patient-controlled analgesia (PCA) postoperatively. After intravenous induction, each patient was intubated with a double -lumen endotracheal tube to accomplish single lung ventilation. During the operation, patients’ vital signs were followed every five minutes throughout the operation. All patients were extubated at the end of surgery and transferred to the ward.
Surgical technique
Patients were placed in lateral decubitus position, with the surgeon and the assistant standing on the abdominal side. The assistant stood at the foot-stool (Figure 1). The entire procedure was performed under the screen observation.

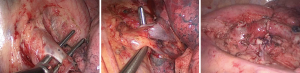
A 3.5 cm incision was made in the anterior axillary line 4th intercostal space (Figure 2) for upper lobe resection and 5th intercostal space for middle and inferior lobe resection. A soft plastic wound protector was applied to the incision without rib-spreading procedure. A 10-mm 30 degree thoracoscope was positioned in the superior side of the incision during the lobectomy. The designed surgical instruments (Figure 3), in together with the harmonic shear (Ethicon Endo-Surgery Inc, Cincinnati, OH, USA) or hook electro-cautery were applied during the procedure.


The bronchus, vein and artery were divided and dissected separately using an endo-linear stapler (Covidien, Mansfield, MA, USA or Ethicon Endo-Surgery Inc, Cincinnati, OH, USA) or ligated by using hem-o-locks (Weck Surgical, Teleflex, Limerick, USA) before dissection. In the cases of lower or middle lobe lesions, the dissection order was vein, artery and bronchus, and in the cases of upper lobe lesions, and the dissection order would be changed to artery, vein and bronchus (Figures 4,5). The specimen was taken out in the specimen bag (Ethicon Endo-Surgery Inc, Cincinnati, OH, USA). Conventionally, systemic mediastinal lymph node dissection was followed after the removal of the target lung. A 28-Fr chest tube was inserted at the end of the operation, and the chest tube would be removed in the cases there was no air leakage and the volume of drainage was less than 200 mL per day 24 hours post-operatively.
Statistical analysis
Clinical data for all patients were collected from the clinical database of our institution by trained surgical coordinators. All data collected was tabulated using Microsoft Excel for further analysis. Statistical analysis was undertaken using SPSS software (SPSS, Inc, Chicago, Ill, version 17.0, USA).
Results
Between October 2013 and February 2014, a total of 54 uniportal VATS lobectomies were attempted in Zhongshan Hospital of Fudan University. Among these cases, there were 51 patients (94.4%) underwent uniportal resection were completed without conversion to multiple incisions or open thoracotomy: an extra port was added for one left upper lobectomy to place the endo-linear stapler through the upper pulmonary vein. One patient with chronic obstructive pulmonary disease (COPD) was converted to four ports approach due to technique difficulty. One patient was converted to mini-thoracotomy to due lymph node sticking to the pulmonary artery. Pathological diagnosis confirmed the lymph node without tumor metastasis.
Of the 51 cases of uniportal lobectomy, the average operation duration was 122.2±37.5 min (90-160 min). Upper lobe resection cost shorter duration than middle or low lobe resection (90.7±41.6 vs. 150.7±34.5 min; P=0.031). The average volume of estimated blood loss was 88.8±47.1 mL (50-200 mL). None of all the 51 patients required blood transfusion. The average number of harvested lymph nodes was 14.9±3.8 [7-23].
Prolonged stay in intensive care unit (ICU) was not recorded among the patients underwent uniportal VATS lobectomy. The median chest tube duration was 2.2 days, ranging from 2 to 9 days. There were eight patients required non-steroidal anti- inflammatory drugs (NSAID) after the removal of epidural analgesia, and five patients continued NSAIDs administration one month after discharge.
Three patients developed complications, including two prolonged air leakages lasting more than 5 days and one atrial fibrillation. There was no perioperative death in this cohort. After the removal of chest tube, all patients were discharged following the confirmation of lung re-expansion by chest X rays. The average length of stay in hospital was 4.6±2.0 days, ranged from 3-10 days.
Discussion
In this study, we retrospectively reviewed the data on uniportal VATS lobectomy in our center. Based on the surgical refinements on the technique and instruments, the uniportal VATS lobectomy showed safety and feasibility in the surgical resection of lung cancer. The results from our single center indicated that uniportal VATS would be an alternative beside conventional VATS lobectomy.
Since introduced in early 1990s, VATS has developed over 20 years from a simple procedure to more complicated operations including lobectomy and esophagectomy. In 2004, Rocco reported the first worldwide uniportal thoracoscopic wedge resection (4). Since then, several articles have confirmed the safety and feasibility of uniportal operation in simple procedure. Undoubtfully, patients would benefit from a surgery with less traumatic manipulations (10-12). Especially when it came to the major operations: Gonzalez-Rivas et al. reported their experience of uniportal lobectomy, which was the world’s first report on uniportal major lung resection. Since then, Gonzalez-Rivas et al. have published serial research relating to uniportal segmentectomy, pneumonectomy, and sleeve lobectomy (8,13,14). The previous experience from the Western medical centers encouraged our attempt on uniportal VATS lobectomy.
Based on the western experience, technical refinements were introduced to the uniportal surgery in our medical center. Firstly, the assistant surgeon stood at the foot-stool, and the shoulder of the assistant was kept in adduction with extended arms throughout the procedure, it would result in better ergonomics in compared with the posture that the shoulder was kept in abduction with both arms flexed (15). Secondly, a wound protector was applied to the incision to avoid iatrogenic contamination to the thoracoscope so that the continuity was assured throughout the uniportal surgery. Thirdly, new surgical instruments were invented to facilitate the uniportal surgery. As the key step of uniportal VATS was to make the angle for the separate dissection of pulmonary root (8), a tiny suction stick with angle was invented to allow more instruments through one single incision. In this report, improved surgical techniques decreased the operative time to an average of 162 min, which was slightly longer in compared with Gonzalez-Rivas’s previous report (16).
Different from the previous report on VATS lobectomy, shorter operation duration was recorded in this cohort when the VATS upper lobectomy was performed (17). In three-hole VATS lobectomy, the upper lobectomy was technically more difficult in compared with the lower lobe dissection. Especially when performing the dissection along the apical branch of pulmonary artery, the iatrogenic injury to the artery was not uncommon and would lead to lethal bleeding during the operation (18). On the contrary, in uniportal VATS lobectomy, the mobilization of apical branch was the first step in dealing with the hilum structure. Located at the 4th intercostal space, the incision was close to the superior border of the superior pulmonary vein, which improved the exposure of apical branch and facilitated the following dissection. In the lower lobectomy, the mobilization of inferior vein would require the assistant surgeon to push the diaphragm and pericardium so that the surgeon could retract the lower lobe. The duration was therefore longer in lower lobe lobectomy in uniportal surgery.
Mediastinal lymph node dissection is another key step of the operation. Though there is debate on the choice of mediastinal lymph node dissection or sampling, we always performed mediastinal lymph node dissection. According to NCCN guidelines, more than three mediastinal lymph node stations were harvested in this cohort. The most difficult part of mediastinal lymph node dissection is the left subcarinal lymph node dissection, which is located deep and hard to be exposed. For left lower lobe (LLL) dissection, we usually dissected the subcarinal lymph node before we cut the left low lobe bronchus. And for left upper lobe dissection, a good method was introduced by Wang (19): a tape was retracted anterior, which was placed through the plane between the left bronchus and the left inferior vein. With this method, subcarinal lymph node dissection became easier in uniportal VATS.
The experience on multi-incision VATS was described as an important step prior to the uniportal surgery (7,20,21). Technically, it would be easier to switch from two ports to single port than from three or four ports to single port (21). However, for those who are familiar with four-port VATS lobectomy, switching from four ports to three ports and then double-port, and sequentially to single port might be time consuming. Meanwhile, in the cases safety would be compromised, additional ports or conversion to open thoracotomy should be considered without hesitation. That explains why the conversion rate was higher in our study than others. On the other hand, the morbidity and mortality rate were close to the previous reports (16).
Previous study convinced that uniportal surgery was associated with less postoperative pain (22). Similar findings were observed in this study, there was very low incidence of NSAID consumption at one month following the operation. As was reported in previous literatures (11), there were 53% routine VATS patients required medications for pain relief, including 26% NSAIDs and 27% narcotics. In this study, the results were promising even when it was not a comparative study on post-operative pain. Further clinical study based on larger population is required to answer this question.
The main limitation of this study was its retrospective design and relatively small sample size. As the number of uniportal VATS was increasing, further studies based on higher evidence level were required to confirm more findings, both surgically and oncologically.
Conclusions
Uniportal VATS lobectomy is safe and feasible. Operative instrument improvement can make uniportal surgery easier. With caution, surgeon can change from four ports to single port.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Swanson SJ, Herndon JE 2nd, D’Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Alar T, Ozcelik C. Single-incision thoracoscopic surgery of pleural effusions for diagnosis and treatment. Surg Endosc 2013;27:4333-6. [PubMed]
- Berlanga LA, Gigirey O. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax using a single-incision laparoscopic surgery port: a feasible and safe procedure. Surg Endosc 2011;25:2044-7. [PubMed]
- Rocco G, La Rocca A, La Manna C, et al. Uniportal video-assisted thoracoscopic surgery pericardial window. J Thorac Cardiovasc Surg 2006;131:921-2. [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [PubMed]
- Feng M, Shen Y, Wang H, et al. Uniportal VATS LUL lobectomy. Asvide 2014;1:359. Available online: http://www.asvide.com/articles/393
- Andreetti C, Menna C, Ibrahim M, et al. Postoperative pain control: videothoracoscopic versus conservative mini-thoracotomic approach†. Eur J Cardiothorac Surg 2014;46:907-12. [PubMed]
- Nicastri DG, Wisnivesky JP, Litle VR, et al. Thoracoscopic lobectomy: report on safety, discharge independence, pain, and chemotherapy tolerance. J Thorac Cardiovasc Surg 2008;135:642-7. [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [PubMed]
- Shen Y, Feng M, Tan L, et al. Thoracoscopic esophagectomy in prone versus decubitus position: ergonomic evaluation from a randomized and controlled study. Ann Thorac Surg 2014;98:1072-8. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Thoracoscopic lobectomy through a single incision. Multimed Man Cardiothorac Surg 2012;2012:mms007.
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]


