Single-staged uniportal VATS major pulmonary resection for bilateral synchronous multiple primary lung cancers
Introduction
Difficulty in diagnosis and treatment decision making for patient with bilateral multiple pulmonary foci usually raises a clinical dilemma for clinicians. An aggressive surgical approach can offer sufficient specimens for diagnostic differentiation and the greatest chance for long-term survival in patient with presumptive synchronous multiple primary lung cancers (SMPLC) (1,2). In such situation, mini-invasive technique of video-assisted thoracoscopic surgery (VATS) has been reported to be effective (1,3,4). Since uniportal VATS has been attempted as a less invasive technique (5), we transferred it into the management of presumptive SMPLC. Here, we present two cases of bilateral SMPLC managed through single-staged uniportal VATS with major pulmonary resection, which provides simplified mini-invasive diagnosis and synchronous treatment.
Cases report
Patient 1 was a 67-year-old female, who was presented with chest pain for about 2 months. Preoperative high-resolution computed tomography revealed four ground glass opacity (GGO) lesions (two in the right upper lobe, each in the left upper and lower lobe, respectively, Figure 1A-D). Patient 2 was a 53-year-old female, who was admitted with a mass in the right upper lobe (Figure 1E) and a GGO lesion in the superior segment of the left lower lobe (Figure 1F). Both of them were presumptively diagnosed with bilateral SMPLC. The preoperative staging work-up indicated no sign of lymphadenopathy or distal metastasis. Given no surgical contraindication, single-staged uniportal VATS for bilateral pulmonary foci was planned for each of them with written informed consent.
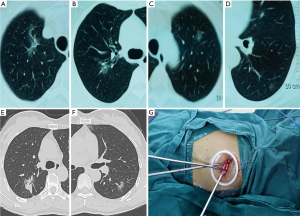
General anesthesia with double-lumen endotracheal intubation was administered to each of them. A 5 mm 30° thoracoscope was used for inspection. Patient 1 was firstly placed in a right lateral decubitus position. On the left, a 3.5 cm incision was made in the fourth intercostal space at the anterior axillary line. Each of the two lesions was identified through digital palpation and the surface of the lung right on the top of each lesion was marked using a suture, which was also used for retraction during resection. Then wedge resections were performed using curved endostaplers with margins ≥2 cm. Frozen-section examination confirmed an adenocarcinoma in the upper lobe and a carcinoma in situ in the lower lobe. One chest tube was placed at the posterior part of the incision. After the left-side operation, the patient was rotated to the opposite side for right upper lobectomy. Cushions were used to lift the patient to avoid kicking or compression to the contralateral chest tube during positioning. On the right, a 4.5 cm incision was made in the fifth intercostal space at the anterior axillary line (Figure 1G). Right upper lobectomy (Figure 2) was performed with the right upper pulmonary vein, arterial branches, bronchus and pulmonary fissures dissected and divided sequentially. Then frozen-section examination confirmed two adenocarcinomas and systematic lymph node (LN) dissection was performed (a total of 7 stations and 15 LNs were harvested). One chest tube was placed at the posterior part of the incision. Patient 2 was also firstly placed in a right lateral decubitus position to undergo left lower lobe superior segmentectomy (Figure 3) via a 4.5 cm incision made in the fifth intercostal space at the anterior axillary line. The superior segmental artery, bronchus, drainage vein, and the intersegmental plane were dissected and divided sequentially. Frozen-section examination confirmed an adenocarcinoma followed by systemic LN dissection (a total of four stations and seven LNs were harvested). After the left-side procedure, she was rotated to the opposite side for right upper lobectomy followed by systemic LN dissection (a total of five stations and seven LNs were harvested) after confirmation of adenocarcinoma by frozen-section examination. Chest tube strategy was the same as did for patient 1. The operation time for patient 1 and 2 were 260 and 285 min, respectively. The intraoperative blood loss of patient 1 and 2 were 30 and 60 mL, respectively. The postoperative courses were both uneventful. Pathological examination documented four primary lung cancers of patient 1 (right upper lobe, two minimally invasive adenocarcinomas, T2aN0M0 and T1aN0M0, respectively; left upper lobe, minimally invasive adenocarcinoma, T1aN0M0; left lower lobe, adenocarcinoma in situ, TisN0M0) and two primary lung cancers of patient 2 (right upper lobe, acinar predominant adenocarcinoma, T1bN0M0; left lower lobe, lepidic predominant adenocarcinoma, T1aN0M0).


Discussion
The common criteria used for differentiating between SMPLC and intrapulmonary metastases depend on the results of pathologic examination and even molecular and genomic analysis (8). However, preoperative diagnosis is often difficult due to difficulty in obtaining sufficient specimens for histological examination whether through bronchoscopy or percutaneous puncture, especially for those small peripheral lesions. Single-staged procedures executed via traditional multiportal VATS have been demonstrated to be feasible and safe for selected patients with bilateral SMPLC (3). Although it may be also reasonable to perform delayed resections for some small GGO lesions with no negative effect on outcomes (9), we prefer to perform single-staged surgery when the lesions are highly suspected of malignancy. Since introduced by Rocco et al. in 2004 (10), sporadic reports on uniportal VATS for lung cancer have been published (5,11,12). Uniportal VATS causes less postoperative pain and fewer paresthesia owing to less intercostal space involved (13). For our patients, it’s hard to procure thorough diagnoses for all lesions through neither bronchoscopy nor percutaneous puncture due to their disperse locations, small sizes, and manifestations of GGO. To simplify the diagnosis and treatment course, we transferred the less invasive technique of uniportal VATS into the management of SMPLC to achieve mini-invasive diagnosis and synchronous treatment. Systemic LN dissection is routinely performed when anatomic pulmonary resection (lobectomy or segmentectomy) is planned in our daily work. But for pure GGO lesions, especially those ≤1 cm, wide wedge resection with adequate free margin seems to be oncologically enough because there is seldom invasiveness or LN involvement (14). Therefore, we didn’t perform LN dissection for the left side of patient 1 while station seven would be dissected from the right side.
This successful attempt first demonstrates the feasibility of simplified mini-invasive diagnosis and synchronous treatment using bilateral uniportal VATS major pulmonary resection for the management of SMPLC with multiple bilateral lesions.
Acknowledgements
Funding: This work was supported by the Key Science and Technology Program of Sichuan Province, People’s Republic of China (2013SZ0005 to L.L.X.).
Disclosure: The authors declare no conflict of interest.
References
- Yu YC, Hsu PK, Yeh YC, et al. Surgical results of synchronous multiple primary lung cancers: similar to the stage-matched solitary primary lung cancers? Ann Thorac Surg 2013;96:1966-74. [PubMed]
- Jung EJ, Lee JH, Jeon K, et al. Treatment outcomes for patients with synchronous multiple primary non-small cell lung cancer. Lung Cancer 2011;73:237-42. [PubMed]
- Mun M, Kohno T. Single-stage surgical treatment of synchronous bilateral multiple lung cancers. Ann Thorac Surg 2007;83:1146-51. [PubMed]
- Mun M, Kohno T. Efficacy of thoracoscopic resection for multifocal bronchioloalveolar carcinoma showing pure ground-glass opacities of 20 mm or less in diameter. J Thorac Cardiovasc Surg 2007;134:877-82. [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- Liu C, Ma L, Lin F, et al. Right upper lobectomy. Asvide 2014;1:264. Available online: http://www.asvide.com/articles/277
- Liu C, Ma L, Lin F, et al. Superior segmentectomy of left lower lobe. Asvide 2014;1:265. Available online: http://www.asvide.com/articles/278
- Xue X, Liu Y, Pan L, et al. Diagnosis of multiple primary lung cancer: a systematic review. J Int Med Res 2013;41:1779-87. [PubMed]
- Gulati CM, Schreiner AM, Libby DM, et al. Outcomes of unresected ground-glass nodules with cytology suspicious for adenocarcinoma. J Thorac Oncol 2014;9:685-91. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. [PubMed]
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol 2014;25:1462-74. [PubMed]


