Effectiveness and safety of a protocolized mechanical ventilation and weaning strategy of COPD patients by respiratory therapists
Introduction
Mechanical ventilation is a common procedure used to treat patients with respiratory failure due to chronic obstructive pulmonary disease (COPD). Although it is life saving, it is invasive, expensive and associated with some serious potential risks such as ventilator associated pneumonia, ventilator induced lung injury, hemodynamic problems and prolonged intensive care unit (ICU) stay. Therefore, reducing the time patients spend on mechanical ventilation will lead to improvements in patient care, decrease in related complications and reduced costs.
Prior research has demonstrated that the use of standardized weaning protocols can shorten the duration of mechanical ventilation (1-4). Assessing readiness to wean and the choice of ventilator strategies and modes vary among physicians, and protocols performed by non-physician medical staff such as nurses and respiratory therapists (RTs) may reduce the total duration of mechanical ventilation and ICU length of stay (5,6). However, these previous studies were performed in mixed medical and surgical patient populations and only evaluated the role of these protocols during the weaning period. Furthermore, there is little data evaluating the effect of implementing these protocols in difficult to wean patients such as COPD (7-9).
In 2011 January, our ICU recruited a RT and implemented a mechanical ventilation and weaning protocol. Prior to this date, the choice of ventilator mode and approach to weaning was left to the discretion of individual respiratory physicians. The aim of this study was to evaluate the impact of this protocol on total duration of mechanical ventilation and weaning, ICU stay, weaning success rates and mortality in COPD patients.
Materials and methods
This cohort study was conducted in the 29-bed ICU of a 450-bed teaching hospital specializing in pulmonary diseases and thoracic surgery. The data of patients who were managed before the implementation of the protocol was collected retrospectively and compared with the prospectively collected data of patients managed with a protocol. We included all COPD patients who required mechanical ventilation due to an exacerbation more than 48 hours. There was no change in the physicians, treatment modalities and other medical staff working in the ICU between the study periods. COPD diagnosis was made according to the Global Initiative for Chronic Obstructive Lung Disease criteria and confirmed by the medical records of our hospital (10). Patients who needed advanced ventilatory techniques (PEEP level greater than 10 cmH2O, inverse ratio ventilation, airway pressure release ventilation, prone positioning) at the beginning or during the follow up period due to acute respiratory distress syndrome were excluded in both intervention and control groups due to the incompatibility with the protocol and the exceptional nature of the disease. Patients with a tracheostomy, who were ventilated shorter than 48 hours, patients with a cause of ICU admission different from COPD exacerbation and patients who were under home mechanical ventilation support were also excluded. The study was approved by the institutional review board (number: 298) and written informed consent was obtained from the patients and/or next of kin.
Protocol-based group
A full time RT was assigned to work in the ICU in January 2011. From that time, a novel protocol-based mechanical ventilation and weaning protocol for our center was developed and pilot tested. After some adjustments, the protocol was initiated for all intubated COPD patients. When an intubated patient was admitted to the ICU or a patient was intubated during ICU stay, the RT set the following parameters and settings: Assisted pressure controlled mode, inspiratory pressure titration to achieve a tidal volume (Vt) of 6-8 mL/kg, minimum respiratory frequency (f) of 15 breaths/min, 3-5 cmH2O of positive end expiratory pressure (PEEP), flow triggering at minimum level but avoiding auto-triggering, inspiratory time (Tinsp) set to maximum 1.5 seconds and fractional inspired oxygen concentration (FiO2) titrated to achieve an arterial oxygen saturation (SaO2) greater than 90% (11). The patients were evaluated at least two times a day and manipulations in Tinsp, f or both were done to achieve a partial arterial carbon dioxide pressure (PaCO2) lower than 50 mmHg and a pH value greater than 7.25. FiO2 levels were decreased gradually until 50%. Patients were assigned for a spontaneous breathing trial (SBT) with a t-piece for 2 hours when they met the following criteria: PaO2/FiO2 >150, PEEP ≤8 mmHg, Glasgow coma score (GKS) >8, number of controlled breaths=0, number of patient triggered breaths ≤35, pH >7.25 or PaCO2 <50 mmHg, mean arterial pressure ≥60 mmHg with no or low doses of vasopressors (≤5 μg/kg/min), adequate cough for airway protection (10). If the patients showed good tolerance with an acceptable arterial blood gas analysis (pH ≥7.35, PaO2/FiO2 >150 with a FiO2 ≤50%, f ≤35 breaths/min), they were extubated. If signs of intolerance occurred (change in neurologic status, f >35 breaths/min, pH <7.32, increase in PaCO2 >10 mmHg, heart rate >140 beats/min, systolic blood pressure >180 or <90 mmHg), patients were re-connected to the ventilator and SBT was repeated the following day (11). If the patients failed the SBT for three consecutive days, then they were switched to pressure support ventilation and weaning was continued by gradual reductions in pressure support level until 7 cmH2O is tolerated as described elsewhere (12,13). If the patients tolerated the SBT with 7 cmH2O of pressure support for 2 hours (with the same tolerability criteria for SBT with a t-piece as above) they were extubated.
Physician-directed group
Before January 2011, the choice of mechanical ventilation mode was made by the physician’s individual preferences. The most common preferred modes were assisted volume controlled ventilation, synchronized intermittent mandatory ventilation, pressure controlled ventilation and pressure support ventilation. Weaning procedures were also determined by the physician in charge of the patient. Weaning criteria were not monitored daily and the assessing readiness to wean and decisions for extubation were also physician directed and performed according to subjective criteria differing among physicians. Specific mechanical ventilation and weaning protocols did not exist, but in general physicians employed commonly recommended procedures such as 2 hours of SBTs with t-piece or 7 cmH2O pressure support.
Definitions
Extubation success was defined as 48 hours independence from mechanical ventilation (invasive or noninvasive). If the patients could never reach the weaning period during hospitalization (deterioration in the clinical status, death etc.) they were classified as non-weaned for the primary analysis. Duration of mechanical ventilation (MV) was defined as the time from intubation until successful extubation. Length of stay (LOS) in ICU was defined as the time from intubation until ICU discharge. Weaning duration was defined as the time from the beginning of the first SBT (either with t-piece or pressure support) until successful extubation.
Statistical analysis
Statistica 8.0 software (StatSoft Inc. Tulsa, USA) was used for the analysis. Continuous variables were expressed as medians with interquartile range (IQR) and categorical variables were expressed as numbers with percentages. Medians were compared by Mann Whitney U test and frequencies were compared by Fisher’s exact test. Kaplan-Meier curves with log rank test were used to compare the time to successful extubation and liberation from mechanical ventilation and time to ICU discharge. Patients who died during ICU follow-up were censored in the primary analysis; rates of deaths in both study periods were compared as a secondary outcome. Cox proportional hazards regression was used to adjust for other factors that can affect MV duration and ICU length of stay. Results were expressed as hazard ratio (HR) with 95% confidence intervals (CIs). A two sided P value of <0.05 was considered as significant.
Results
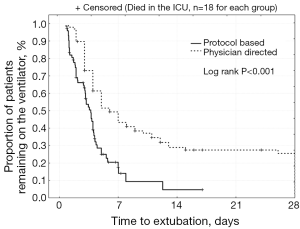
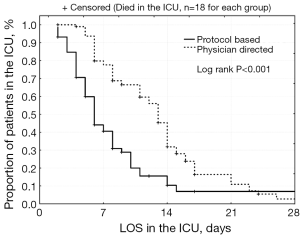
Seventy three patients were enrolled in the protocol based RT directed group and compared with 97 patients in the physician directed group (Table 1). Patients in the protocol based RT directed group were significantly older with a significantly higher median APACHE II score. Weaning success rates were comparable between the two groups (72% vs. 68%, P=0.52). When the non-weaned patients were excluded from the analysis, extubation success rate was significantly higher (94% vs. 78%, P=0.014) in the protocol based RT directed group. Mortality rates were comparable between the two groups (Table 2). Time to successful liberation from mechanical ventilation was significantly shorter in the protocol based RT directed group (Figure 1). MV duration until the first SBT (2.8 vs. 3 days, P=0.018), weaning duration (2 vs. 26 hours, P<0.001), total MV duration (3.1 vs. 5 days, P<0.001) and LOS in the ICU (6 vs. 12 days, P<0.001) were also significantly shorter in the protocol based RT directed group (Table 2, Figure 2). Overall, patients in the protocol based group were more likely to become liberated from mechanical ventilation when compared with the physician directed group (unadjusted HR: 2.06 with 95% CI: 1.44-2.95, P<0.001) We included the a-priori specified variables in a multivariable Cox-proportional hazard model to evaluate the adjusted likelihood of becoming liberated from mechanical ventilation. Age, APACHE II, PaCO2 and weaning outcome were selected as covariates for the main effect model (purposeful selection). MV duration until the first SBT, weaning duration and LOS in ICU were significantly correlated with total MV duration so they were not included in the model. Model check using Kolmogorov-Smirnov test was performed and all the variables included in the model were normally distributed. There were no colinearities between covariates. The only factors shortening total MV duration was found as being in the protocol based group (HR: 2.08, 95% CI: 1.40-3.10, P<0.001) and extubation success (HR: 1.87, 95% CI: 1.13-3.08, P=0.015) after adjusting for age, APACHE II and PaCO2 levels just before intubation.
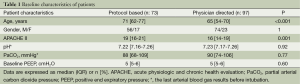
Full table
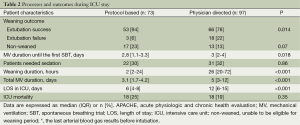
Full table
Discussion
This study suggests that the implementation of mechanical ventilation and weaning protocol directed by a respiratory therapist can reduce both weaning and total MV duration and LOS in the ICU in COPD patients. The impact of the RT directed protocol remained the same after adjusting for some probable confounding factors such as age, APACHE II and PaCO2. Moreover, this kind of practice may improve the weaning success rates in this patient group for whom weaning can often be difficult and prolonged.
It is a well-known fact that intubation and mechanical ventilation have some very important potential risks in addition to obvious benefits. Ventilator associated pneumonia, probably the most common complication of intubation occurs at a rate of 1% to 3% per day of mechanical ventilation (14). These complications lead to increased costs and mortality in ICU patients. For this reason, reducing the duration of MV and ICU stay has always been an important aim for critical care physicians.
Selection of mechanical ventilation mode is often based on clinician familiarity and institutional preferences since there is a paucity of evidence indicating that choice of mode affects clinical outcome. In an observational study enrolling 412 ICUs in eight countries, the most commonly used ventilator modes were assisted controlled ventilation, synchronized intermittent mandatory ventilation, pressure support ventilation and pressure controlled ventilation. Tidal volumes were set around 8-9 mL/kg, respiratory rate around 12-15 breaths/min and PEEP around 5 cmH2O (15). There are studies reporting that this variety of decisions made by physicians during follow up and weaning period may lead to prolonged MV duration and ICU stay (16). Therefore, we decided to use a standard ventilation mode and weaning protocol for all patients.
Our findings are consistent with other studies that have implemented weaning protocols. Tonnelier et al. reported that a weaning protocol directed by nurses instead of physicians resulted in a 6 days of shortening in MV duration and ICU stay in a combined group of ICU patients which included COPD patients. However, the improvements in COPD patients did not reach statistical significance (5). In another study performed by Wood and colleagues on cardiac surgery patients, a progressive increase in the proportion of patients weaned by the RTs and a slight decrease in total ventilation time and weaning duration was observed (3). Marelich et al. reported a decrease in MV duration from median 124 hours to 68 hours for a mixed group of ICU patients of which 16 were COPD in their randomized controlled study (6). Ely et al. also reported a significant decrease in weaning and total MV duration with a weaning protocol including daily screening of patients’ respiratory functions (17). In a recently published meta-analysis, Blackwood et al. reported that weaning protocols decreased the mean duration of mechanical ventilation by 25%, duration of weaning by 78% and ICU stay by 10% (16). These findings were consistent with our results. Moreover, we detected a significant decrease also in the duration of MV until first SBT. This finding also supports the importance of a mechanical ventilation protocol including daily screening and assessing readiness to wean according to some objective criteria.
Weaning outcomes vary among studies. Esteban et al. reported 82% of extubation success with SBT with t-piece in a combined group of patients of which 21% were COPD (13). Lower success rates around 65% are also reported in some other studies (18). These alterations might be due to the experience of the ICU staff, severity or the patients and differences in the ventilation and weaning modes used in different centers. Our extubation success rate was consistent with the literature in the physician directed group whereas it was significantly higher in the Protocol based RT directed group. There is also some evidence that weaning protocols may increase the extubation success rates. Teixeira et al. reported an increase in extubation success around 17% with a weaning protocol (19). This is probably due to the strict protocol used for assessing readiness to wean patients in protocol group. This finding also suggests that the alterations in the physicians’ individual decisions to extubate the patients might worsen the success rates as reported in some other studies (2).
To our knowledge, this is the first study that evaluates the impact of non-physician directed mechanical ventilation “plus” weaning protocol beginning from the intubation until extubation in adults in a developing country. Hermeto et al. performed a similar study in premature infants and reported outcomes consistent with our study (20). Nevertheless, our study has several limitations. First, because of the non-randomized design, the two groups compared may not be comparable although we have performed a regression analysis. We only could compare the APACHE II score for the severity of the disease because other indices like pulmonary function tests were not available for all patients. Second, the idea that things get better over time regardless of what we do might have an impact on the positive results in the intervention group. Even though the unit staff remained the same throughout the study period, their skills could have improved with experience. Although protocols are helpful in improving outcomes in the ICU, we must take into account that every patient is unique and sometimes it may not be possible to follow protocols for each patient. An experienced physician and a vigilant nurse who perform a once daily SBT may have a big role to play in the successful weaning of mechanically ventilated patients. It may not be cost effective to recruit a respiratory therapist if ICU physicians perform the mechanical ventilation and weaning protocols but because of the lack of intensivists in most of the centers throughout the world, non-physician medical staff such as nurses or respiratory therapists able to perform these protocols may decrease the workload of intensivists. Last but not least, this study enrolled a homogenous patient group in a single center so the results are not generalizable to other patient groups and centers.
Conclusions
This study demonstrated that, a simple mechanical ventilation and weaning protocol applied by non-physician ICU staffs like respiratory therapists might improve weaning success and shorten the total duration of mechanical ventilation and ICU stay in COPD patients requiring mechanical ventilation over a 48-hour period. These improvements may also be achieved without a change in mortality rates. Further multi-centric studies are needed to evaluate the impact of these protocols on heterogeneous patient groups in different centers.
Acknowledgements
The authors would like to thank the American Thoracic Society’s MECOR (Methods in Epidemiologic, Clinical and Operations Research) Program, and Damon Scales MD, in particular, for stimulating their interest in this research and advice on the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Horst HM, Mouro D, Hall-Jenssens RA, et al. Decrease in ventilation time with a standardized weaning process. Arch Surg 1998;133:483-8; discussion 488-9. [PubMed]
- Kollef MH, Shapiro SD, Silver P, et al. A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med 1997;25:567-74. [PubMed]
- Wood G, MacLeod B, Moffatt S. Weaning from mechanical ventilation: physician-directed vs a respiratory-therapist-directed protocol. Respir Care 1995;40:219-24. [PubMed]
- Davies N. Nurse-initiated extubation following cardiac surgery. Intensive Crit Care Nurs 1997;13:77-9. [PubMed]
- Tonnelier JM, Prat G, Le Gal G, et al. Impact of a nurses’ protocol-directed weaning procedure on outcomes in patients undergoing mechanical ventilation for longer than 48 hours: a prospective cohort study with a matched historical control group. Crit Care 2005;9:R83-9. [PubMed]
- Marelich GP, Murin S, Battistella F, et al. Protocol weaning of mechanical ventilation in medical and surgical patients by respiratory care practitioners and nurses: effect on weaning time and incidence of ventilator-associated pneumonia. Chest 2000;118:459-67. [PubMed]
- Kirakli C, Ozdemir I, Ucar ZZ, et al. Adaptive support ventilation for faster weaning in COPD: a randomised controlled trial. Eur Respir J 2011;38:774-80. [PubMed]
- Duan J, Tang X, Huang S, et al. Protocol-directed versus physician-directed weaning from noninvasive ventilation: the impact in chronic obstructive pulmonary disease patients. J Trauma Acute Care Surg 2012;72:1271-5. [PubMed]
- Hill NS. Following protocol: weaning difficult-to-wean patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001;164:186-7. [PubMed]
- MacIntyre NR, Cook DJ, Ely EW Jr, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 2001;120:375S-95S. [PubMed]
- García Vicente E, Sandoval Almengor JC, Díaz Caballero LA, et al. Invasive mechanical ventilation in COPD and asthma. Med Intensiva 2011;35:288-98. [PubMed]
- Alía I, Esteban A. Weaning from mechanical ventilation. Crit Care 2000;4:72-80. [PubMed]
- Esteban A, Alía I, Gordo F, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1997;156:459-65. [PubMed]
- George DL. Epidemiology of nosocomial pneumonia in intensive care unit patients. Clin Chest Med 1995;16:29-44. [PubMed]
- Esteban A, Anzueto A, Alía I, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 2000;161:1450-8. [PubMed]
- Blackwood B, Alderdice F, Burns KE, et al. Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev 2010;CD006904. [PubMed]
- Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 1996;335:1864-9. [PubMed]
- Robriquet L, Georges H, Leroy O, et al. Predictors of extubation failure in patients with chronic obstructive pulmonary disease. J Crit Care 2006;21:185-90. [PubMed]
- Teixeira C, Maccari JG, Vieira SR, et al. Impact of a mechanical ventilation weaning protocol on the extubation failure rate in difficult-to-wean patients. J Bras Pneumol 2012;38:364-71. [PubMed]
- Hermeto F, Bottino MN, Vaillancourt K, et al. Implementation of a respiratory therapist-driven protocol for neonatal ventilation: impact on the premature population. Pediatrics 2009;123:e907-16. [PubMed]


