Nodular fasciitis on chest wall in a teenager: a case report and review of the literature
Introduction
Chest wall tumors rarely occur in childhood, accounting for only 1.8% of the solid tumors in the chest wall (1). The ribs are the most common site of chest wall tumors, but the clavicle, sternum, scapula and soft tissues are also involved. Sarcomas make up for the majority of chest wall tumors, and benign tumors, such as eosinophilic granuloma, aneurysmal bone cyst, hamartoma, osteoma, osteochondroma, and chondroma are rarer than malignant tumors.
Nodular fasciitis is a benign, rapid proliferation of fibroblasts and myofibroblasts in the subcutaneous tissues and resembles malignant soft tissue sarcomas from a clinical and pathologic point of view (2).
Its rapid growth, abundant cellularity, and mitotic activity often lead to a misdiagnosis of sarcoma. Nodular fasciitis is relatively common in the adult population; however, it is rarely reported chest wall tumor among children (3).
We report a rare case of nodular fasciitis in a 15-year-old boy that developed in the wall of his chest.
Case report
A 16-year-old boy presented with a palpable mass on his left anterior chest wall at the level of the fifth intercostal space. The mass had first been noticed 2 months ago and had grown rapidly. The patient denied any history of trauma, infection, or tuberculosis. On the physical examination, a hard, round and smooth-surfaced mass that was affixed to the chest wall was palpated. The skin over the lesion was neither tender nor hot.
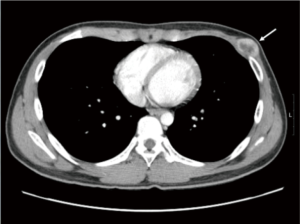
The chest X-ray and bone scan showed no abnormal findings. The chest computed tomography scan revealed a well-enhanced ovoid mass approximately 3 cm × 2 cm in size in the anterior portion of the patient’s left lower chest wall (Figure 1). The central portion of this mass showed poor enhancement, while the peripheral portions showed intense enhancement. To obtain a pathologic confirmation and to manage the mass, surgical resection was decided. The mass was located between the pectoralis muscle and the ribs. Its exterior surface was well demarcated by the pectoralis muscle, but the interior surface was firmly attached to the periosteum of the ribs, intercostal muscles and fascia. The mass was completely resected, including the intercostal muscles and surrounding soft tissues.
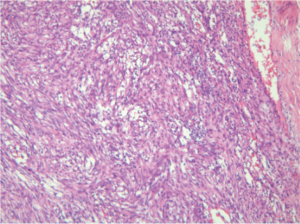
The mass had a hypercellular pattern, and upon microscopic examination, short and irregular bundles of spindle cells with microhemorrhage and inflammatory cells were noted. However, intermittent myxoid and hypocellular areas were also observed and mitotic activity was not found (Figure 2).
The patient recovered without any complications and remains free of recurrence 2 years after surgery.
Discussion
Nodular fasciitis is a benign mesenchymal tumor that often presenting as a rapidly growing soft tissue mass. It can be easily mistaken for a malignancy because its clinical and histologic characteristics are similar to malignancies such as sarcoma (4).
Nodular fasciitis was first described by Konwaler et al. in 1955 and was initially named pseudosarcomatous fibromatosis. Other terms, such as pseudosarcomatous fasciitis, infiltrative fasciitis, and proliferative fasciitis, have also been used synonymously. Price et al. (5) first used the term “nodular fasciitis” because the origin of tumor was from the superficial and deep fascial layers.
Nodular fasciitis is most commonly observed in young adults between 20 and 40 years of age (6,7). Approximately 10% of the lesions occur in children (7). Although men and women equally affected, in childhood, the lesions may occur predominantly in boys.
The lesions are generally small and solitary and commonly appear in the upper extremities in adults. After the upper extremity, the next most common site of involvement is the lower extremity, with only 9% located in the chest wall. In infants and children, the head and neck are commonly involved.
Bemrich-Stolz et al. reported 18 cases of nodular fasciitis in children (8), 7 of which occurred in the head and neck, 5 in the upper and lower extremities, and 5 in back. The average age was 9 years, with a range of 5 months to 18 years; the male gender was predominant (72%). All lesions were solitary.
Nodular fasciitis has characteristic pseudosarcomatous features and is generally considered to be a benign and a reactive fibroblastic growth. Nodular fasciitis is a benign myofibroblastic proliferation that usually occurs in the subcutaneous tissues of the upper extremities, and trunk, as well as in the head and neck of young adults. Most patients present with a rapidly growing painless solitary mass. Grossly, the masses are solid, nodular, rubbery, or firm.
Nodular fasciitis is subdivided into three types based on their predominant histological features: myxoid (type 1), cellular (type 2), and fibrous (type 3) (5,9). Type 1 lesions are composed of spindle, plump or stellate fibroblast-like cells embedded in myxomatous stroma rich in hyaluronidase-digestible acid mucopolysaccharide. This type demonstrates an abundance of immature capillaries running in a parallel direction, frequent red cell extravasation and considerable inflammatory changes. Type 2 lesions have a higher cellularity and less plentiful ground substances. The fibroblast-like spindle cells have been revealed to be large and plump with vesicular nuclei. Type 3 lesions are characterized by an increased collagen production, and fibroblast-like cells are more slender and spindle-shaped. Nodular fasciitis may have a variable histologic appearance, depending on the preoperative duration of the lesion, and a correlation between histological patterns and clinical features has been suggested (5,9). The histological appearance of nodular fasciitis may change in time from active myxoid to cellular, before changing lastly to the mature fibrous type. The myxoid type of nodular fasciitis should be differentiated from the myxoid variant of malignant fibrous histiocytoma, which usually occurs in older patients and forms a large tumor. The cellular type of fasciitis can easily be mistaken for a sarcoma, while the fibrous type may be confused with other benign lesions.
Surgical excision is treatment of choice. These lesions rarely recur and sometimes even slowly regressed (8); furthermore, they do not metastasize and are readily cured by local excision.
Nodular fasciitis may be misdiagnosed as a sarcoma due to its rapid growth, abundant cellularity, mitotic activity and poorly circumscribed nature. A previous study demonstrated that recurrent nodular fasciitis was often a misdiagnosed malignancy (10). While spontaneous resolution after fine needle aspiration has reported, surgical excision should be considered because of its potential diagnostic confusion with sarcoma, a rare incidence in the pediatric population, and its minimal morbidity during surgical excision.
Although nodular fasciitis is rare among chest wall tumor of the pediatric population (11), it should be considered during the evaluation of chest wall tumors in childhood for an accurate diagnosis and proper intervention.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Kumar AP, Green AL, Smith JW, et al. Combined therapy for malignant tumors of the chest wall in children. J Pediatr Surg 1977;12:991-9. [PubMed]
- Wagner LM, Gelfand MJ, Laor T, et al. A welcome surprise: nodular fasciitis presenting as soft tissue sarcoma. J Pediatr Hematol Oncol 2011;33:316-9. [PubMed]
- Tomita S, Thompson K, Carver T, et al. Nodular fasciitis: a sarcomatous impersonator. J Pediatr Surg 2009;44:e17-9. [PubMed]
- Di Serafino M, Maurea S, Vallone G. Nodular fasciitis of the chest: case report of a rare presentation. Musculoskelet Surg 2011;95:251-3. [PubMed]
- Price EB Jr, Silliphant WM, Shuman R. Nodular fasciitis: a clinicopathologic analysis of 65 cases. Am J Clin Pathol 1961;35:122-36. [PubMed]
- Stout AP. Pseudosarcomatous fascitis in children. Cancer 1961;14:1216-22. [PubMed]
- Allen PW. Nodular fasciitis. Pathology 1972;4:9-26. [PubMed]
- Bemrich-Stolz CJ, Kelly DR, Muensterer OJ, et al. Single institution series of nodular fasciitis in children. J Pediatr Hematol Oncol 2010;32:354-7. [PubMed]
- Shimizu S, Hashimoto H, Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology 1984;16:161-6. [PubMed]
- Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer 1982;49:1668-78. [PubMed]
- Mazura JC, Matrai C, Spigland N, et al. Intramuscular nodular fasciitis of the rectus abdominis muscle in an 11-year-old girl. Skeletal Radiol 2013;42:147-50. [PubMed]


