An anterior mediastinal mass: delayed airway compression and using a double lumen tube for airway patency
Introduction
Induction and management of general anesthesia in patients with a mediastinal mass can be challenging and cases related to mediastinal masses have been continuously reported (1-3). For a patient’s safety, anesthesiologists and cardiothoracic surgeons need to evaluate the pathophysiologic consequences of mediastinal masses and cooperate closely.
A careful preoperative evaluation of thoracic structures and stepwise induction of anesthesia, including initiating cardiopulmonary bypass (CPB) with continuous monitoring of ventilation and hemodynamics, are essential. This is particularly the case in high risk patients with a mediastinal mass related signs, symptoms, or radiologic findings such as severe postural symptoms, stridor, cyanosis, tracheal compression (>50%) or with associated bronchial compression, pericardial effusion or superior vena cava syndrome (4-6). Intermediate risk patients who have mild to moderate symptoms and/or tracheal compression (<50%) are also assessed and perioperative care plan should be planned for airway security. In contrast, low risk patients who are asymptomatic or mildly symptomatic, without postural symptoms or radiologic findings of significant compression of structures, endure ordinary general anesthesia (6,7).
This report describes delayed compression of the airway after uneventful induction of anesthesia occurred even in a low risk patient who was not expected to show any airway compromises. This report also showed how to resolve it with a rather simple technique: using a double lumen tube (DLT) and fiberoptic bronchoscope (FB) as a possible solution to maintain airway patency.
Case report
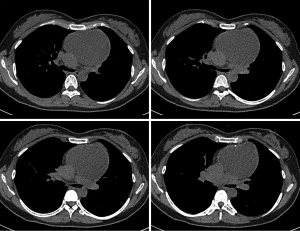
A 35-year-old previously healthy female (163 cm/58 kg) presented for excision of an anterior mediastinal mass, found incidentally on a chest radiograph taken as part of a routine checkup. She had no signs or symptoms related to the mass such as cough, chest pain, superior vena cava obstruction, hoarseness, syncope, dysphagia, dyspnea; or noisy breathing at rest, on exertion, in the supine position, or during sleep. Her chest X-ray and computed tomography (CT) scan, which were taken one day before surgery, suspected a teratoma (7.5 cm × 9.2 cm × 14 cm) in the left anterior to middle mediastinum, compressing the brachiocephalic vein, but did not show any airway compromise (Figures 1,2).

A median sternotomy and surgical excision of the mediastinal mass was planned. The cardiothoracic surgeon and the anesthesiologist agreed to perform stepwise induction of anesthesia without initiation of CPB because the patient did not show any preoperative airway compromise related to the anterior mediastinal mass (low risk).
The patient was transferred to the operating room premedicated with 0.2 mg glycopyrrolate. Routine anesthetic monitoring was applied. Induction was achieved with an initial dose of 50 mg propofol followed by two times of 30 mg. The patient’s spontaneous mask ventilation was maintained without any respiratory difficulties. Seventy five mg succinylcholine was administered to achieve tracheal intubation. A size 7.0 cuffed endotracheal tube was placed easily via direct laryngoscopy demonstrating a Cormack-Lehane grade I view with concomitant placement of a right radial arterial catheter. FB (PortaView-LFTM, Olympus Medical Systems Corp., Tokyo, Japan) revealed no compression of the trachea or both main bronchi. Bilateral breathing sounds and bilateral chest expansion were also confirmed and 4 mg of vecuronium was then administered.
Sevoflurane and remifentanil were used to maintain anesthesia. A central venous catheter was placed in the right internal jugular vein without difficulty. The elapsed time was about 20 minutes from the beginning of induction to central venous catheterization.
At this time, the peak inspiratory pressure began to increase to over 40 cmH2O. Breathing sounds from the left lung diminished considerably and chest wall expansion was limited. Arterial saturation began decreasing despite manual ventilation with continuous positive airway pressure and 100% oxygen was added. After placing the patient in the left lateral decubitus and the intermittent oxygen flush via FB which was pushed distal to the compressed part of the left main bronchus, oxygen saturation started to increase.
FB revealed total compression of the left main bronchus and partial compression of the carina. The entire length of the left main bronchus was, however, not compressed (less than 2 cm) and the left upper and lower lobar bronchi were intact (Figure 3); thus, we considered to re-intubate with a left-sided DLT (32 Fr. MallinckrodtTM Endobronchial tube, Covidien, Tullamore, Ireland) expecting the rigid DLT to maintain airway patency.
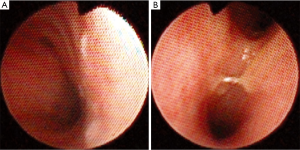
Preparation for emergent CPB started after the patient was laid in the supine position. At the same time, the endotracheal tube was withdrawn, and the trachea was intubated using a DLT via direct laryngoscopy. We inserted the FB into the bronchial lumen and introduced the DLT and FB from the trachea to the left main bronchus, and further into the distal border of the compressed site with the FB as a guide. We were able to place the DLT in the appropriate position to prevent compression of the carina and left main bronchus. After the FB was withdrawn, the DLT was connected to the ventilator and conventional mechanical ventilation was initiated. FB revealed that the tip of the right lumen did not enter the left main bronchus. Bilateral breathing sounds were clearly auscultated. The elapsed time was 3 minutes during the procedure. The plan for emergent CPB was rediscussed and then canceled.
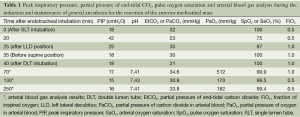
On median sternotomy, a round mass with a smooth margin was found located in the left anterior to middle mediastinum and was compressing the carina, left main bronchus, and brachiocephalic vein. The mass was totally removed with minimal blood loss. End-tidal carbon dioxide and peak inspiratory pressure remained within the normal range and ventilation was kept stable through surgery (Table 1). FB was performed frequently to access airway patency. After relieving the airway, the DLT was replaced with a size 7.0 cuffed endotracheal tube.
Full table
At the end of the operation, the patient was extubated uneventfully. She did not show any difficulties breathing in the post-anesthetic care unit. No injuries on the trachea and bronchus caused by the mediastinal mass and DLT were present intraoperatively and postoperatively. The histopathological diagnosis confirmed the mass as a mature teratoma.
Discussion
Anesthetic management of patients with anterior mediastinal masses is very complicated. Clinicians should look for any symptoms such as cough, dyspnea on exertion, chest pain, fatigue, or vocal cord paralysis (4,5). A careful evaluation of the size and the location of the mass are important for predicting the physiological effects it will have on surrounding mediastinal and other thoracic structures (8). Based on this information, an anesthetic plan should be formulated prior to induction of anesthesia. This is, however, particularly the case in intermediate to high risk patients with a mediastinal mass related signs, symptoms, or radiologic findings (4-6).
In contrast, low risk patients such as our patient tolerate ordinary general anesthesia (6,7). Our patient did not have any signs and symptoms related to the mediastinal mass and the CT scan showed that the airway was intact; thus, stepwise induction with propofol and succinylcholine was performed. FB revealed that airway patency was maintained after tracheal intubation; therefore, vecuronium was given. However, this patient showed delayed compression of the airway after induction of anesthesia. It means that clinicians should pay attention to low risk patients as well as intermediate and high risk patients.
This compression seemed to be related to the anesthetic agents and muscle relaxants that trigger a decrease in respiratory muscle tone, producing reduced lung volume and loss of the outward force of the chest. Furthermore, anesthetic agents relax the airway smooth muscle; thus, the airway is compressed more easily (9-12). Hemorrhage inside the mass after needle biopsy or a rapid-growing mass may compress the airway as well. However, our patient’s chest X-ray and CT scan were taken one day before surgery and a needle biopsy had not been performed. Internal jugular vein catheterization was also unlikely to cause the airway compression, because there were not any difficulties during catheterization.
When ventilatory difficulties ensue after induction of anesthesia, reported management options include repositioning the patient, placing rigid bronchoscope distal to the obstruction, or initiating CPB (4,8). When our patient’s oxygenation level began to be compromised, repositioning her in the left lateral decubitus was life-saving. We decided that a rigid bronchoscope was not necessary because the FB slid smoothly through the compressed part of the left main bronchus, and repositioning the patient was effective for oxygenation.
A DLT is usually intended for one lung ventilation but in this case, with the help of FB, we used it like a rigid stent that opened up the compressed carina and left main bronchus as we pushed the tip distal to the obstruction. The DLT was rigid enough to push away the mass even in the supine position. Even though the airway in this case was maintained with a DLT, DLT intubation was not our first choice because our patient had a low risk of airway compromises and DLT intubation causes more frequent complications such as sore throat, hoarseness, vocal cords injuries, and tracheobronchial injuries (13,14).
To use a DLT, several limitations should be considered. First, use of a DLT is an option for some patients with masses externally compressing the carina or bronchus, it is not an option, however, for patients with intrinsic airway tumors. Second, the nature of the mass may also influence the successful insertion of a DLT. Solid mass may be difficult to move. In this case, CT scans indicated that the mass was not so hard. Third, a DLT cannot be a possible solution to maintain airway patency if the main bronchus is entirely collapsed. The present patient showed that the length of the collapsed left main bronchus was only 2 cm and the left upper and lower lobar bronchi were intact. Fourth, because the right main bronchus is shorter than the left main bronchus, it may be much more difficult to place a DLT in a patient with compression of the right main bronchus. Lastly, this procedure is not for patients with hemodynamic compromise.
Positioning the patient for DLT intubation was also considered. It was possible to intubate a DLT in the lateral position. However, we positioned the patient in the supine position because intubation in the supine position is easier and if needed, repositioning the patient in the lateral position could relieve airway compression.
In conclusion, even though patients may not have any preoperative signs, symptoms, or radiologic findings related to an anterior mediastinal mass, and the airway is secured after uneventful induction of anesthesia, these do not guarantee that airway patency is maintained during surgery. Therefore, anesthesiologists and cardiothoracic surgeons have to prepare for delayed compression of the airway, even in low risk patients. Using a DLT in patients undergoing or expected to be in ventilatory jeopardy due to anterior mediastinal masses during induction of anesthesia is a possible solution to maintain airway patency.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Tauro LF, Shetty P, Kamath A, et al. Double whammy - mediastinal and ovarian teratoma: a rare clinical co-existence. J Thorac Dis 2012;4:434-6. [PubMed]
- La Mantia E, Franco R, Rocco R, et al. Spindle cell lipoma: a rare tumor of the mediastinum. J Thorac Dis 2013;5:E152-4. [PubMed]
- Tan PC, Esa N. Anesthesia for massive retrosternal goiter with severe intrathoracic tracheal narrowing: the challenges imposed -A case report-. Korean J Anesthesiol 2012;62:474-8. [PubMed]
- Slinger P, Karsli C. Management of the patient with a large anterior mediastinal mass: recurring myths. Curr Opin Anaesthesiol 2007;20:1-3. [PubMed]
- Tempe DK, Arya R, Dubey S, et al. Mediastinal mass resection: Femorofemoral cardiopulmonary bypass before induction of anesthesia in the management of airway obstruction. J Cardiothorac Vasc Anesth 2001;15:233-6. [PubMed]
- Blank RS, de Souza DG. Anesthetic management of patients with an anterior mediastinal mass: continuing professional development. Can J Anaesth 2011;58:853-9, 860-7. [PubMed]
- Béchard P, Létourneau L, Lacasse Y, et al. Perioperative cardiorespiratory complications in adults with mediastinal mass: incidence and risk factors. Anesthesiology 2004;100:826-34; discussion 5A.
- Atlee JL. eds. Complications in Anesthesia (Second Edition). Philadelphia: WB Saunders;2006:670-2.
- Bergman NA. Reduction in resting end-expiratory position of the respiratory system with induction of anesthesia and neuromuscular paralysis. Anesthesiology 1982;57:14-7. [PubMed]
- Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 2005;31:1327-35. [PubMed]
- Neuman GG, Weingarten AE, Abramowitz RM, et al. The anesthetic management of the patient with an anterior mediastinal mass. Anesthesiology 1984;60:144-7. [PubMed]
- Dikmen Y, Eminoglu E, Salihoglu Z, et al. Pulmonary mechanics during isoflurane, sevoflurane and desflurane anaesthesia. Anaesthesia 2003;58:745-8. [PubMed]
- Ceylan KC, Kaya SO, Samancilar O, et al. Intraoperative management of tracheobronchial rupture after double-lumen tube intubation. Surg Today 2013;43:757-62. [PubMed]
- Gilbert TB, Goodsell CW, Krasna MJ. Bronchial rupture by a double-lumen endobronchial tube during staging thoracoscopy. Anesth Analg 1999;88:1252-3. [PubMed]


