Septic shock with tension fecothorax as a delayed presentation of a gunshot diaphragmatic rupture
Introduction
Diaphragmatic rupture (DR), due to penetrating injury, is relatively infrequent, but it is even more rarely that it represents a life-threatening situation. Sennertus in 1541 described the first diaphragmatic injury with abdominal organ herniation and subsequently, Riolfi performed the first successful repair in 1886 (1). In 1951 this injury was well understood and delineated, as shown by Carter’s publication (2) of the very first series of cases.
There is a significant probability that the diagnosis of acute DR may be delayed or remain missed during the initial diagnostic assessment of the wounded. Late diagnosis is often associated with herniation of abdominal contents into the thorax (3). The reported incidence of DRs due to thoraco-abdominal trauma is 0.8-5% (4) and up to 30% of diaphragmatic hernias are identified as late clinical presentations (5).
The injury of the diaphragm is the result of a fall from a significant height or high energy blunt or penetrating thoracoabdominal trauma (6). Concomitant injuries of other organs are usually present in cases of DR (1).
Road traffic accidents (RTAs) are identified as the cause of DRs in 80-90% of blunt trauma cases. In penetrating trauma, the firearm injuries are categorized as Low (muzzle velocity of less than 600 m/sec, e.g., handguns’ projectiles) or High velocity injuries (muzzle velocity of more than 600 m/sec, e.g., military or hunting weapons’ projectiles) (7). Another specific form of penetrating injuries is stab wound with a very high incidence compared with wounds from firearms in some countries.
We hereby present a case of a late clinical manifestation of a life threatening acute event of colonic strangulated hernia and perforation inside the left hemithorax 15 whole years after the high velocity gunshot DR (Grade III, according to AAST, American Association for the Surgery of Trauma), which also caused paraplegia to the patient.
Case presentation
Α 43-year old male, former police officer, with a history of paraplegia, obesity and multiple gunshot wounds to the spinal cord during a conflict 15 years before, was urgently transferred from a provincial hospital into the emergency department of our hospital in a moribund state with severe septic shock, severe respiratory distress and accompanying symptoms of acute abdomen. Upon admission the patient’s oxygen saturation was <85% and he was spontaneously breathing with excessive dyspnoea whilst in supine position and with some improvement of the dyspnoea in the sitting position. The patient reported that the sudden onset of his symptoms had occurred 48 hours earlier.
During the primary assessment in emergency department the patient was breathless with 29 breaths/min and he had heart rate 140/min, arterial pressure 90/60 mmHg, breathe sounds decreased on the left side, chest pain at rest and on palpation in the left hemithorax and upper abdomen with strong evidence of peritonaism. Laboratory investigations revealed remarkable signs of severe sepsis as:
- Arterial blood gases showed severe respiratory acidosis: pH =7.198, PCO2 =55.0 mmHg, PO2 =75.0 mmHg, HCO3– =20.9 mmol/L, Base Excess = –7.8 mmol/L (Deficit), O2 Sat =89%;
- Full blood count: Hct =48.9%, Hb =16.5 gr/dL, pronounced neutrophilic leukocytosis WBC =37×103/μL [normal range (4.2-11)×103/μL] with neutrophills 89.1%, CRP =29.3 mg/dL (normal range <0.5 mg/dL);
- Chest radiograph demonstrated the presence of intestinal loops in left pleural cavity, and the potential appearance of hydropneumothorax or pyothorax with concomitant deviation of the trachea towards the right side (Figure 1).
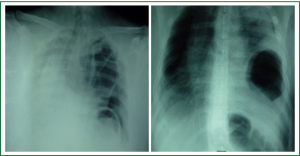
A diagnosis of DR was immediately suspected, with the possibillity of strangulated and perforated herniating colon, inside the left hemithorax.
Abdominal and chest computed tomography (CT) scan was not feasible to be carried out because of his unstable haemodynamic status (minimally controllable by inotropic support and because of his respiratory failure and inability to breathe whilst in the supine position (O2 Sat =82%); Therefore, the patient had to be taken at once to the operating theatre for emergency left thoracotomy and laparotomy.
Intraoperative findings were not just plain “Empyema thoracis”, but “Faecothorax” with the intrathoracic presence of strangulated, perforated transverse colon through rupture of the left hemidiaphragm and a defect of the left hemidiaphragm, measuring 6 cm, whose edge was adherent to the colonic wall (implying a chronic condition of diaphragmatic hernia with very likely cause of DR from gunshot trauma 15 years earlier).
Intraoperatively the thoracic cavity was thoroughly cleaned from the feces and the gangrenous omentum which was adherent to the pericardium was mobilized (firmly adherent to the pericardium, chest wall and both pulmonary lobes). The surgical intervention included also: (I) resection of the necrotic portion of the transverse colon and reduction of the viable part of it into the peritoneal cavity through the traumatic defect of the left hemidiaphragm; (II) repair of the defect of the hemidiaphragm by sewing in two layers (first layer with interrupted non-absorbable sutures, second layer with continuous absorbable suture); (III) insertion of a basal, No 36 intercostal chest drain; (IV) temporary transverse colostomy.
The patient stayed in the Intensive Care Unit during the first 30 postoperative days, because he needed mechanical ventilation, inotropic support and multivalent antibiotic treatment for his most severe septic condition. Then he remained as an in-patient in a surgical Ward for an additional fortnight.
He was finally discharged home on 45th postoperative day with his chest drain connected to a Portex ampulatory chest-draining bag. The chest drain was gradually withdrawn by 2.5 cm every 2 weeks and it was finally completely removed on 3rd postoperative month. The bowel continuity was also restored at the same time (3rd postoperative month) with an uneventful postoperative course.
Discussion
Although the reported incidence of DR is between 0.8% and 5%, its diagnosis is often missed in 7-66% of blunt trauma cases (8). In 4-6% of patients undergoing surgery for trauma, concomitant diaphragmatic injuries are present (9). Blunt trauma is usually caused by sudden deceleration (RTAs and falls) while penetrating trauma is often due to injuries from fireguns and miscellaneous stabbing weapons (knives etc.). Approximately 75% of DRs are caused by blunt and 25% by penetrating trauma.
In cases of penetrating trauma to the lower chest, DRs were present in 15% of stab and in 46% of gunshot wounds (9). More generally diaphragmatic injuries account for about 65% of thoracoabdominal penetrating trauma (10). The DR may be direct, due to an impalement or missile which crosses the abdomen to the chest and vice versa.
In cases of blunt trauma, the DR is caused by a sudden and excessive Increase of the ever present gradient of pressures between the abdominal cavity (always positive pressure) and the pleural one (always negative pressure); Therefore, this excessive increase of pressures’ gradient overcomes the consistency and integrity of the diaphragmatic tissue. The blunt DR usually causes radial tears in the diaphragm, while penetrating injuries are indicated by small holes that follow the size of the projectile (10).
Possible explanations for the delayed onset of this 6 cm large diaphragmatic hernia of this case, is the creation of tissue defect because of the inflammatory change of the initially devitalized diaphragmatic muscle, or a delayed diagnostic detection of an initially large defect which was happened only after the herniation occurred (1). However there is still a report by Grimes, relating to the late onset of DR which records three phases of DR with over many years which eventually results in intrathoracic herniation and strangulation of the viscera within the chest (11).
The most cephalad anatomic location of the diaphragm may lie as high as the 4th thoracic dermatome (T4) on the right side and the 5th dermatome (T5) on the left during expiration. The most caudad location of the diaphragm is the 8th thoracic dermatome during deep inspiration; The lowest posterior point of the diaphragm is attached to the 12th ribs. Therefore the diaphragm is vulnerable to become ruptured in any case penetrating injury sustained in the anatomic region between T4 and T12.
In our case the patient had a spinal injury at the T10 level, which was responsible for his paraplegia and DR (12).
Not only the blunt, but also the penetrating trauma is more usually associated with left-sided DR rather than with right-sided one. One explanation for this is the assumption of a frontal assault, during which a right-handed assailant causes a left-sided penetrating injury. On the other hand, the protecting role of the liver is crucial in small right-sided diaphragmatic injuries as it tamponades the defect preventing bowel herniation (13).
Even though the real mechanism of blunt or penetrating DR remains speculative, three are the dominant theories: (I) shearing of a stretched diaphragmatic membrane; (II) avulsion of the diaphragm from its points of attachment; and (III) sudden force transmission through viscera acting as a viscous fluid (9). Regarding blunt injury there have been described more mechanisms like the position of the glottis at the time of accident, the direct injury from a fractured rib etc(14).
Initially the trauma patient may have no symptoms or signs that could indicate a diaphragmatic injury. In some cases the presence of severe, more “apparent” concomitant injuries may lead to the misdiagnosis of the DR.
Over time the traumatic deficit is enlarged, and herniation of abdominal organs becomes more likely, particularly if left-sided. According to a small series of delayed diagnosis of DR, 3 out of 16 patients (19%) had their DR missed at initial laparotomy, while the majority (15 cases out of 16) were on the left side (13,15).
Our patient had suffered from serious constipation for many years, but two days before his admission he felt a sudden episode of chest and abdominal pain and dyspnoea, that was worsening till the time of admission.
Patients usually present with non-specific symptoms and may complain of chest or abdominal pain, dyspnoea, tachypnoea and cough or hiccup (singultus) (8,14). Other symptoms reported are haematemesis due to splenic vein thrombosis and varices of gastric fundus from a herniated thoracic spleen, and pneumopericarditis (16).
Studies indicate that about 12-69% of cases are not diagnosed preoperatively (16). Bowel sounds audible in the thorax are indicated as a shift of gut content through a traumatic diaphragmatic hernia while chest radiography is the first-line imaging modality with a diagnostic sensitivity of 46% on the left and 17% on the right side (17-19).
In case that the herniated content is the stomach, the insertion of a nasogastric tube increases the diagnostic sensitivity of radiography in 75% (19). Helical CT with saggittal, axial and coronal sections shows diagnostic sensitivity of 56-87% and specificity of 75-100%, whereas multidetector CT 71-90% and 98-100% respectively (14).
It was impossible to carry out a CT scanning due to excessive oxygen desaturation in the supine position. A possible explanation for this is a unilateral diaphragmatic paralysis, characterized by worsening dyspnoea: in the supine position the abdominal viscera enter deeper or higher into the pleural cavity, driven only by the pressures’ gradient alone, i.e., without the gravity’s force opposing the aforementioned gradient. This results in a significant (>500 mL) positional decrease in vital capacity and oxygen saturation (20).
The surgical management often includes hernia reduction, pleural drainage and repair of the diaphragmatic defect. Laparotomy or thoracotomy or laparoscopy or thoracoscopy are the surgical options that may be used.
Diligent investigation of DR through an open laparotomy or diagnostic laparoscopy has a crucial role especially if the overall haemodynamic and respiratory status of the patient allows the second surgical approach (18).
It is remarkable that the mortality is only low in cases of elective surgical repairs, however the mortality increases as high as 80% in cases of gangrenous, perforated bowel secondary to strangulation (21,22).
In conclusion, since there are few literature reports related with tension fecothorax, awareness of this rare, life-threatening situation would be valuable for the medical community (23). We could also highlight the difficult diagnostic and therapeutic approach and the late presence of this rare diaphragmatic hernia as a consequence of serious injuries from firearms, characterised by smaller diaphragmatic rents which are more likely to be missed compared with blunt trauma which typically causes large radial tears.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Meyers BF, McCabe CJ. Traumatic diaphragmatic hernia. Occult marker of serious injury. Ann Surg 1993;218:783-90. [PubMed]
- Carter BN, Giuseffi J, Felson B. Traumatic diaphragmatic hernia. Am J Roentgenol Radium Ther 1951;65:56-72. [PubMed]
- Disler DG, Deluca SA. Traumatic rupture of the diaphragm and herniation of the liver. Am Fam Physician 1992;46:453-6. [PubMed]
- Rossetti G, Brusciano L, Maffettone V, et al. Giant right post-traumatic diaphragmatic hernia: laparoscopic repair without a mesh. Chir Ital 2005;57:243-6. [PubMed]
- Pappas-Gogos G, Karfis EA, Kakadellis J, et al. Intrathoracic cancer of the splenic flexure. Hernia 2007;11:257-9. [PubMed]
- Goh BK, Wong AS, Tay KH, et al. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. CJEM 2004;6:277-80. [PubMed]
- Lichte P, Oberbeck R, Binnebösel M, et al. A civilian perspective on ballistic trauma and gunshot injuries. Scand J Trauma Resusc Emerg Med 2010;18:35. [PubMed]
- Shreck GL, Toalson TW. Delayed presentation of traumatic rupture of the diaphragm. J Okla State Med Assoc 2003;96:181-3. [PubMed]
- Shah R, Sabanathan S, Mearns AJ, et al. Traumatic rupture of diaphragm. Ann Thorac Surg 1995;60:1444-9. [PubMed]
- American College of Surgeons. National Trauma Data Base 2000-2004.
- Grimes OF. Traumatic injuries of the diaphragm. Diaphragmatic hernia. Am J Surg 1974;128:175-81. [PubMed]
- Young RL, Page AJ, Cooper NJ, et al. Sensory and motor innervation of the crural diaphragm by the vagus nerves. Gastroenterology 2010;138:1091-101.e1-5.
- Mallory W, Frankel HL, Turnage R. Recognition and management of diaphragmatic injury in adults. In: Ros BD. eds. Up To Date, Wellesley, MA, 2012.
- Desir A, Ghaye B. CT of blunt diaphragmatic rupture. Radiographics 2012;32:477-98. [PubMed]
- Feliciano DV, Cruse PA, Mattox KL, et al. Delayed diagnosis of injuries to the diaphragm after penetrating wounds. J Trauma 1988;28:1135-44. [PubMed]
- Wani AM, Al Qurashi T, Rehman SA, et al. Massive haematemesis due to strangulated gangrenous gastric herniation as the delayed presentation of post-traumatic diaphragmatic rupture. BMJ Case Rep 2010;2010:bcr0420102874.
- Rashid F, Chakrabarty MM, Singh R, et al. A review on delayed presentation of diaphragmatic rupture. World J Emerg Surg 2009;4:32. [PubMed]
- Gelman R, Mirvis SE, Gens D. Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. AJR Am J Roentgenol 1991;156:51-7. [PubMed]
- Dosios T, Papachristos IC, Chrysicopoulos H. Magnetic resonance imaging of blunt traumatic rupture of the right hemidiaphragm. Eur J Cardiothorac Surg 1993;7:553-4. [PubMed]
- Goldman L, Schafer AI. eds. Goldman’s Cecil medicine. 24th Edition. Philadelphia: Elsevier/Saunders, 2012.
- Christie DB 3rd, Chapman J, Wynne JL, et al. Delayed right-sided diaphragmatic rupture and chronic herniation of unusual abdominal contents. J Am Coll Surg 2007;204:176. [PubMed]
- Pross M, Manger T, Mirow L, et al. Laparoscopic management of a late-diagnosed major diaphragmatic rupture. J Laparoendosc Adv Surg Tech A 2000;10:111-4. [PubMed]
- Vermillion JM, Wilson EB, Smith RW. Traumatic diaphragmatic hernia presenting as a tension fecopneumothorax. Hernia 2001;5:158-60. [PubMed]


