Bone metastases with nerve root compression as a late complication in patient with epithelial pleural mesothelioma
Introduction
MPM is an uncommon neoplasm that arises of the pleura and is strongly related to asbestos exposure. A significant increase in the incidence of pleural mesothelioma is expected in the next years. Symptoms are commonly due to local invasion of pleura and mediastinal structures. The most common presenting symptoms are chest pain, shortened of breath and cough. Tumor tend to spread through the pleural cavity and to the chest wall, as well as to the regional lymph nodes in the axilla and supraclavicular area. Distant metastases by hematogenous spread are estimated occur in more than 10% of cases at late stage of the disease (1). The most frequent involved organs beings the liver, adrenal gland, kidney and contralateral lung. Reported cases of bone metastases are rare and the vast majorities are postmortem findings (2-6). The current case describes MPM that involved multiples bones in the progression of disease.
Case
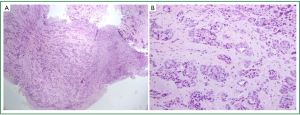
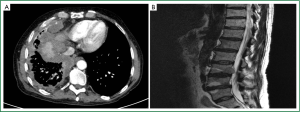
A sixty seven years no-smoker man with previous history of asbestos exposure was admitted to hospital on February 2010 with dyspnea and thoracic pain. Computed tomography (CT) scan showed right pleural effusion and diffuse pleural thickening (Figure 1). At thoracoscopy, multiple pleural nodes in parietal and visceral pleural were found. The biopsy results showed the morphological and immunohistochemical features consistent with the diagnostic of epithelial mesothelioma (Figure 1). The patient initiated chemotherapy with cisplatin and pemetrexed and after four cycles the CT showed stable disease but treatment was stopped due to fatigue. Eight months later patient developed worsened of dyspnea and CT showed progression of pleural disease. At this time patient initiated another line of chemotherapy (vinorelbine), but two months later there was pleural progression with rib affectation causing thoracic pain. Palliative radiotherapy and supportive care were performed. One month later patient was admitted in the hospital because of increasing thoracic pain of difficult control. Analgesic were initiated with improve symptoms, but later patient referred weakness in left leg without abnormalities in the neurologic exam. A bone back magnetic resonance (MRI) was performed showing multiple metastasis lesions to the thoracic and lumbar vertebrae and nerve root involvement compression in L3 (Figure 2). Repose and corticoid were initiated but over the next days the patient continued deteriorate and died 18moths after the original diagnosis of mesothelioma.
Discussion
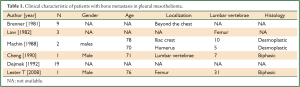
Metastases of MPM are rarely detected and occur at late stage. Series studies have found distant metastases in more than 10% of cases (1). The most commonly involved sites of metastatic are lungs, diaphragm, liver, kidneys, and adrenal glands. Involvement of bone is generally caused by direct extension to the ribs, sternum and thoracic vertebrae, but distant metastases to bone is relatively unusual (Table 1).
Full table
In a review of 123 patients with pleural mesothelioma in one center, nine patients had bone metastases, one at diagnoses and eight during the course of the disease (2). In another series of 115 cases of MPM with postmortem findings available in 60 cases, distant metastases were detected in 39 patients and bone metastases were diagnosed during life in three patients, all of them with sarcomatoid subtype (3). In a full autopsy study during a 10 year period in a single center, bone metastases were found in 19 of 53 pts MPM, engagement of the ribs by direct overgrowth of tumor not included (4). Tumor extension to the spinal cord is uncommon in patients with pleural mesothelioma and usually occurs by direct extension.
The patient in this case presented with known history of MPM and the bone metastases developed in progression of primary tumor. Multiple bone metastases were detected in the MRI, however, the patient remained asymptomatic of these lesions until the metastases developed pain due to nerve compression.
In our case, in agreement with others reports, distant bone metastases were detected late at the disease. However, our patient had epithelial subtype, and distant metastasis have been reported more frequently in sarcomatoid type than epithelial forms of mesothelioma.
Conclusions
Patient with previous exposure to asbestos was diagnosed of pleural mesothelioma and developed distant bone metastases several months after the diagnoses. The expected increase in the incidence of MPM and better survival means this complication may be observed more commonly in the future.
Acknowledgements
Disclosure: All the authors indicate none financial or another interest that is relevant to the subject matter under consideration in this article.
References
- Sussman J, Rosai J. Lymph node metastasis as the initial manifestation of malignant mesothelioma. Report of six cases. Am J Surg Pathol 1990;14:819-28.
- Brenner J, Sordillo PP, Magill GB, et al. Malignant mesothelioma of the pleura: review of 123 patients. Cancer 1982;49:2431-5.
- Law MR, Hodson ME, Heard BE. Malignant mesothelioma of the pleura: relation between histological type and clinical behaviour. Thorax 1982;37:810-5.
- Cheng WF, Berkman AW. Berkman. Malignant mesothelioma with bone metastases. Med Pediatr Oncol 1990;18:165-8.
- Machin T, Mashiyama ET, Henderson JA, et al. Bony metastases in desmoplastic pleural mesothelioma. Thorax 1988;43:155-6.
- Lester T, Xu H. Malignant pleural mesothelioma with osseous metastases and pathologic fracture of femoral neck. Appl Immunohistochem Mol Morphol 2008;16:507-9.


